Credit: A. KITTERMAN, Science Signaling {2019) DOI: 10.1126/scisignal
No matter the pathogen—virus, bacterium or fungus—many “pick a
specific type of lock” on the surface of cells, which allows the microbe
to break and enter into the inner sanctum of the host’s genome.
In a sweeping analysis on how microbes hack into cells and commandeer
them, Australian microbiologists say they are also uncovering
mechanisms in common between microbes and
cancer cells. Their research suggests that in the not-too-distant future it may be possible to cure infectious diseases with repurposed
cancer drugs,
medications that can function across a broad range of pathogens,
eliminating the need for antibiotics, antivirals and antifungals.
An ultimate hope, these scientists say, is ushering in the era of
anti-infectives, drugs that block a vulnerable port of entry for
infectious agents.
Writing in the journal
Science Signaling, Dr. Gholamreza
Haqshenas of Monash Biomedicine Discovery Institute in Australia, and
Dr. Christian Doerig, also of Monash, as well as RMIT University in
Australia, say a radically diverse group of pathogens have surprisingly
evolved to subvert cells in a sly way.
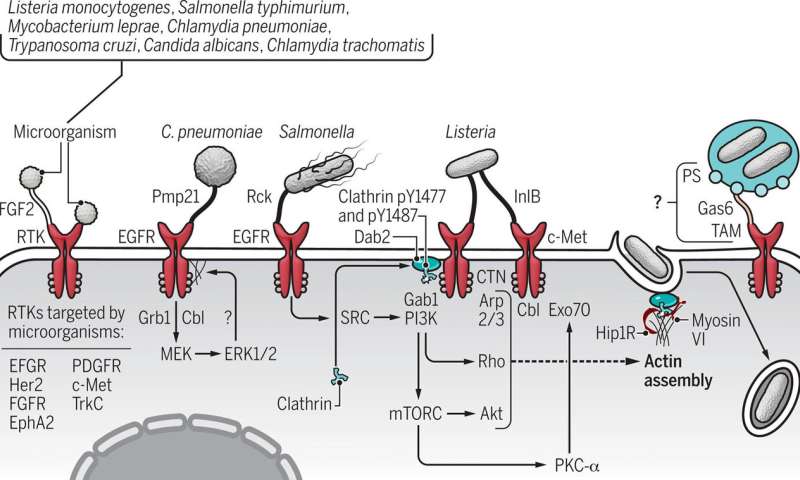
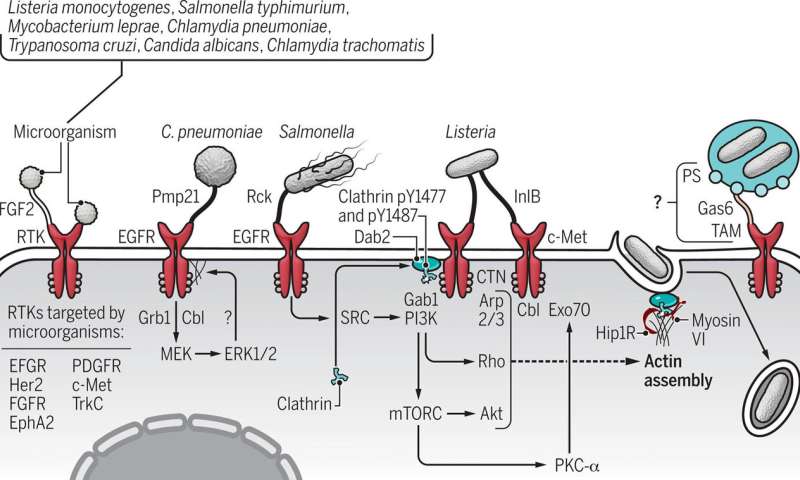
While there are numerous pathways to infection, many microbes enter
their hosts by hijacking signaling proteins, a finding that has become
increasingly clear in recent years, Haqshenas and Doerig say.
Signaling proteins are molecules that are responsible for sending
messages within and between cells. These proteins have segments above
and below the cell surface, which are critical to cellular function. So
it should come as no surprise, the Australian team says, that microbes
responsible for some of the most serious infections have targeted a
superfamily of signaling molecules—receptor tyrosine kinases—as their
route into the host’s cellular domain.
Haqshenas said a vast range of pathogens have evolved mechanisms to
hack into cells by targeting receptor tyrosine kinases, or RTKs. These
microbes can bind to the receptor and like a safe cracker, “unlock” the
cell.
“To name some important ones: Hepatitis C and
influenza viruses,” Haqshenas told Medical Xpress. “Among bacteria, Salmonella and Listeria monocytogenes; and among fungi, Candida albicans.”
When a bacterium, such as Chlamydia pneumoniae binds to a receptor
tyrosine kinase protein on a cell’s surface, the pathogen not only
commandeers the cell, it stimulates signaling, the messages that control
the cell. The pathogen assumes command of everything including the
cell’s structure, its cytoskeleton, thereby easing its entry into the
cell.
The RTK superfamily, which has about 58 members, function as the cell receptors for numerous biological growth factors, such as
epidermal growth factor, platelet-derived
growth factor and
vascular endothelial growth factor,
to name a few. These factors are like keys that once bound to the
receptor can unlock it and enter the cell. An overabundance of RTKs
occurs in some cancers, which can lead to cancer progression. RTK
blockers, medications referred to as small-molecule drugs, have been
developed to treat a form of leukemia and a rare intestinal cancer,
which are marked by excessive RTKs. Gleevec was the first
drug developed in this class and was approved by the U.S. Food and Drug Administration nearly two decades ago.
Although Haqshenas and Doerig report that a veritable rogue’s gallery of viruses can commandeer
receptor tyrosine kinases as an entryway into cells, Doerig underscored “there are other mechanisms of entry for some bacteria.”
Pathogens that use the RTK route to infection have evolved
specialized mechanisms that have allowed them to hack their way into
host cells via this passageway.
For example, Chikungunya, Ebola, Eastern equine encephalitis and
Japanese encephalitis viruses enter cells via RTKs. In addition,
cytomegalovirus, dengue,
herpes simplex virus 1,
human papillomavirus,
Lassa, Marburg, respiratory syncytial, yellow fever, West Nile and Zika
viruses break and enter through the receptor tyrosine kinase pathway.
The list is longer still, according to Haqshenas and Doerig, who say
it also includes Kaposi’s sarcoma-associated herpesvirus, lymphocytic
choriomeningitis, Rose River and vaccinia viruses, pathogens that also
preferentially hack their way into host cells by unlocking RTKs.
“The commonality of relying on the same RTKs suggests that selective
inhibitors against specific RTKs may have broad spectrum anti-infective
properties. Definitely worth further investigation,” Doerig said.
Haqshenas likewise sees their new analysis as a springboard to
further research that explores the possibility of using existing drugs
in new ways against infectious agents.
“Our review highlights the importance of RTKs in the biology of many
pathogens of importance to public health,” Haqshenas said. “Currently,
RTKs are common targets of anti-cancer drugs. The review highlights that
FDA-approved anti-cancer drugs can be repurposed for the treatment of
infections caused by a wide range of
pathogens that must enter host
cells to complete their life cycle.
“This approach will significantly reduce the cost of anti-infective
drug development, and, because a cellular protein is targeted, it
reduces the chance of drug resistance,” Haqshenas said.
More information: Gholamreza Haqshenas et al. Targeting of host cell receptor tyrosine kinases by intracellular pathogens,
Science Signaling {2019)
DOI: 10.1126/scisignal.aau9894