The Solv mobile app will allow patients to find and book urgent care appointments.
SOLV
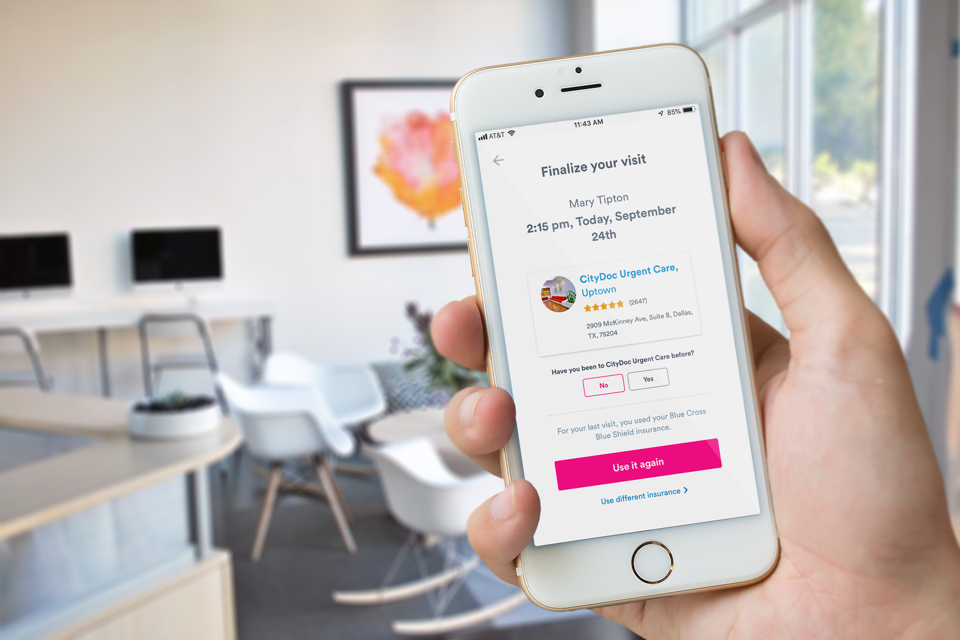
San Francisco-based Solv, a digital startup that helps its customers book same-day urgent care appointments, announced Tuesday that it has launched a mobile app that can help consumers not only book appointments but navigate their health insurance as well.
“Millennials find their healthcare insurance more confusing than their taxes,” says Heather Fernandez, CEO and cofounder of the company.
When consumers download the app, now available for iOS and coming to Google Play later this year, they’ll be given the opportunity to upload their health insurance information into it. Once that’s done, they’ll be able to see at a glance how much of their deductible they’ve used, what expenses they can anticipate for an upcoming appointment and other aspects of their coverage. The app also highlights discounts for things like gym memberships that are available through their insurance.
The app also incorporates the company’s Web functionality—meaning that if consumers face a need for urgent care, the app will let them find a conveniently located center they can book for same-day appointments and determine whether that care is covered by insurance. That’s important, says Fernandez, because according to a survey Solv commissioned about consumer interaction with healthcare, 56% of people have skipped visiting the doctor over a health concern because it was inconvenient to book an appointment.
Solv cofounder and CEO Heather Fernandez
PETER SAMUELS
Fernandez and her cofounder, Daniele Farnedi, are no strangers to bringing digital convenience to older industries. Before founding Solv, both were executives at real estate startup Trulia. After Trulia was acquired by Zillow in 2015, the two decided to take their expertise to healthcare, founding Solv in 2016. “It was a different category but a very similar insight: The consumer experience is terrible,” Fernandez says. The company has raised over $21 million in venture funding from backers such as Greylock and Benchmark ventures.
The company may have struck a chord with consumers. According to Fernandez, more than 8 million people have booked urgent care appointments through Solv this year, up from 2.7 million in the prior year. Last year, it also launched a product that allows people to pay their medical bills from their mobile phones. According to the survey the company commissioned, 14% of its customers would have taken a much more costly trip to the ER rather than urgent care if it hadn’t been for Solv. The company estimates this represents $200 million in saved costs to patients.
For consumers, there’s no cost to using Solv. The company earns its revenue directly from healthcare providers, whom it works with on software, digital communications, bill pay and other services. Looking forward, Fernandez says that the company will expand its offerings still further, enabling consumers to manage more of their healthcare through the platform.
“What we have done as part of our growth is to expand more of our services,” says Fernandez. “More and more people are focused on access to consumers and cost savings.”