As always, the Keynote Address is always a highly anticipated talk GU
ASCO, and this year Dr. David Penson from Vanderbilt University
provided an overview of financial toxicity and quality of among oncology
patients.
Dr. Penson started by highlighting the goals of any new treatment for
cancer, as quoted from Dr. Ian Tannock: We want the patient to live
longer and better, and in the end what matters to patients is overall
survival and quality of life. Defining quality of life is challenging as
there are numerous definitions available in the literature but none
that do a great job of capturing the concept. The National Cancer
Institute’s definition of quality of life is “the overall enjoyment of
life” – not exactly easy to measure. A relevant model to help define
health-related quality of life is provided by Dr. Penson in the
following figure:

The taxonomy of financial hardship in cancer is comprised of three arenas:
- Material conditions: for example, out-of-pocket expenses, missed work, reduced/lost income, and medical debt/bankruptcy
- Psychological response: for example, feeling of distress due to
costs of cancer care, and concern about wages/income meeting expenses
related to costs of cancer care
- Coping behaviors: for example, taking less of or skipping medication or delaying or missing a physician visit
Dr. Penson’s goals for his presentation are to (i) introduce the
concept of financial toxicity in cancer therapy and make people aware of
the negative impact this has on all patient-centered outcomes, and (ii)
to review the financial toxicity of common GU malignancies. He hopes
that we will be aware of the negative effects of financial toxicity of
our therapies on quality of life, and that this will generate a desire
to start a discussion with our patients around the cost of treatment and
a willingness to understand their non-clinical financial situation.
Furthermore, he hopes we think twice before ordering costly
interventions which may have little impact on clinical course but large
impact on the patient’s finances and quality of life.
The scope of the financial burden is that out-of-pocket costs are a
side effect of medical care. In a study of data from the 2011 National
Cancer for Health Statistics, Americans <65 years of age noted that
40-50% had financial burden from medical care, and was still 20-25% in
those ≥65 years of age.
1 Specific to financial toxicity of
cancer survivors, data from the 2013-2016 National Health Interview
Survey suggests that 16-27% of patients have problems paying their
medical bills, 44-52% are worried about paying medical bills, and 9-14%
delayed medical care secondary to financial worries. In Dr. Penson’s
opinion, these data are only going to get worse.
When looking further at the median monthly out of pocket expenses,
Dr. Penson highlighted a 2013 pilot study assessing the financial
toxicity of cancer treatment.
2 Among 254 participants, Zafar
et al. conducted baseline and follow-up surveys regarding the impact of
health care costs on well-being and treatment among cancer patients who
contacted a national copayment assistance foundation along with a
comparison sample of patients treated at an academic medical center.
There were 75% of patients that applied for drug copayment assistance.
Forty-two percent of participants reported a significant or catastrophic
subjective financial burden, 68% cut back on leisure activities, 46%
reduced spending on food and clothing, and 46% used savings to defray
out-of-pocket expenses. Shockingly, to save money, 20% took less than
the prescribed amount of medication, 19% partially filled prescriptions,
and 24% avoided filling prescriptions altogether. Annual out-of-pocket
costs do not fare much better. Among 1,409 Medicare beneficiaries
(median age, 73 years [IQR 69-79 years]; 46.4% female and 53.6% male)
diagnosed with cancer, the type of supplementary insurance was
significantly associated with mean annual out-of-pocket costs incurred
after cancer diagnosis:
3
- $2116 among those insured by Medicaid
- $2367 among those insured by the Veterans Health Administration
- $5976 among those insured by a Medicare health maintenance organization
- $5492 among those with employer-sponsored insurance
- $5670 among those with Medigap insurance coverage
- $8115 among those insured by traditional fee-for-service Medicare but without supplemental insurance coverage
For Medicare beneficiaries, the Affordable Care Act (ACA) will close
the Part D coverage gap (doughnut hole), which will reduce cost sharing
from 100% in 2010 to 25% in 2020 for drug spending above $2,960 until
the beneficiary reaches $4,700 in out-of-pocket spending. To assess this
impact, Dusetzina and Keathing
4 used the Medicare July 2014
Prescription Drug Plan Formulary, Pharmacy Network, and Pricing
Information Files from the Centers for Medicare & Medicaid Services
for 1,114 stand-alone and 2,230 Medicare Advantage prescription drug
formularies. The average price per month for included medications was
$10,060 (range, $5,123 to $16,093). In 2010, median beneficiary annual
out-of-pocket costs for a typical treatment duration was $12,160 (IQR
$12,102 to $12,262) for sunitinib. With the assumption that prices
remain stable after the doughnut hole closes, beneficiaries will spend
approximately $2,550 less. As such, out-of-pocket costs for Medicare
beneficiaries taking orally administered anticancer medications are high
and will remain so after the doughnut hole closes.
According to data from UNC Chapel Hill, financial toxicity is a
possible cause of poor compliance. In a study of 134 bladder cancer
patients, 33 (24%) endorsed financial toxicity (defined as “to pay more
for medical care than you can afford”). Participants who were younger (p
= 0.02), black (p = 0.01), reported less than a college degree (p =
0.01) and had noninvasive disease (p = 0.04) were more likely to
report financial toxicity.
5 Patients who
endorsed financial toxicity were more likely to report delaying care
(39% vs 23%, p = 0.07) due to the inability to take time off work or
afford general expenses. Furthermore, those
with financial toxicity reported worse physical and mental health (p =
0.03 and <0.01, respectively), and lower cancer specific health
related quality of life (p = 0.01), physical well-being (p = 0.01) and
functional well-being (p = 0.05). In a study looking at the impact of
cancer on a patient’s net worth and debt, Gilligan et al.
6
assessed 9.5 million estimated new diagnoses of cancer from 2000-2012.
At two years after diagnosis, 42.4% depleted their entire life’s assets,
with higher adjusted odds associated with worsening cancer, requirement
of continued treatment, demographic and socioeconomic factors (ie,
female, Medicaid, uninsured, retired, increasing age, income, and
household size), and clinical characteristics (ie, current smoker, worse
self-reported health, hypertension, diabetes, lung disease). The
average losses were $92,098. At four years past diagnosis, financial
insolvency extended to 38.2%, with several consistent socioeconomic,
cancer-related, and clinical characteristics remaining significant
predictors of complete asset depletion.
Financial toxicity also affects general quality of life. Data from
the 2011 Medical Expenditure Panel Survey suggested that among 19.6
million cancer survivors (1,329 patients completed the survey), 28.7%
reported at least one financial problem.
7 Furthermore, 7.6%
borrowed money, 11.5% could not afford to cover the cost of medical care
visits, and 20.9% worried about paying their medical bills. Financial
toxicity is also associated with worse survival. Looking at data from
the Western Washington SEER registry (1995-2009) linked to federal
bankruptcy records, patients who filed for bankruptcy were more likely
to be younger, female, and nonwhite, to have local- or regional- (vs
distant-) stage disease at diagnosis, and have received treatment.
8
After propensity score matching, 3,841 patients remained in each group
(bankruptcy v no bankruptcy). The adjusted hazard ratio for mortality
among patients with cancer who filed for bankruptcy versus those who did
not was 1.79 (95% CI, 1.64-1.96). Hazard ratios varied by cancer type,
including colorectal, prostate, and thyroid cancers with the highest
hazard ratios. Importantly, excluding patients with distant-stage
disease from the models did not have an effect on results.
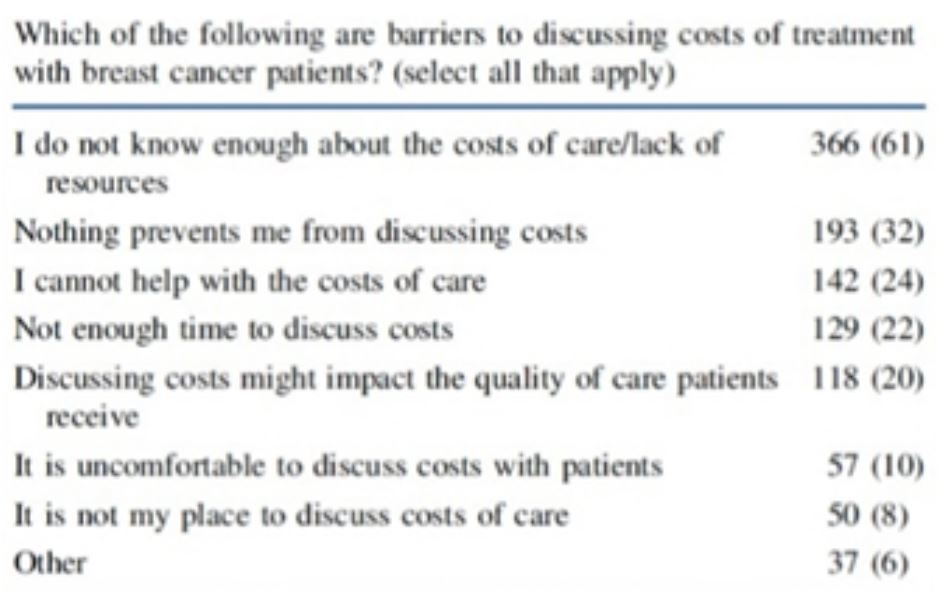
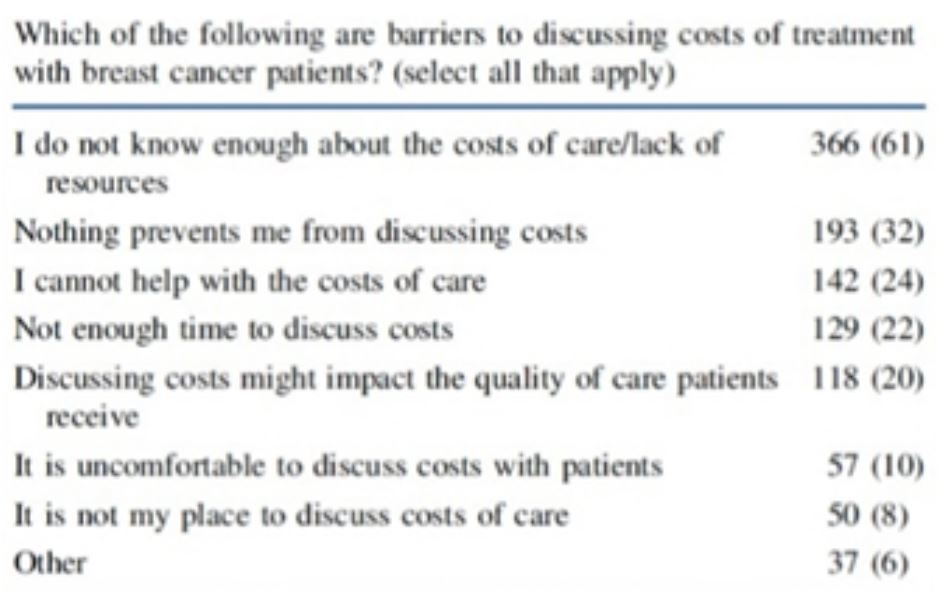
According to Dr. Penson, we have an opportunity to communicate costs
to our patients. Looking at the breast cancer literature, 2,293 members
of the American Society of Breast Surgeons were surveyed, with a 25%
response rate [9]. Shockingly, only 6% of providers included
out-of-pocket costs among the top three most influential factors in
clinical decision making. As follows is the reasons for why providers
were hesitant to discuss the impact of out-of-pocket cost:
Summarizing the financial toxicity among all cancer patients, Dr. Penson highlighted the following points:
- The scope of the problem is greater than many providers appreciate
- Patients cope by avoiding necessary care to save money, and/or going into debt
- Financial toxicity has a negative impact on other clinical outcomes
- Cost communication is not routinely part of the doctor-patient interaction
- We need to start by: acknowledging the problem, learning more about
costs so we can inform our patients, begin a discussion of financial
toxicity with patients, and include financial toxicity as a potential
adverse event in future studies and in shared decision-making
discussions.
Dr. Penson then discussed the highlighted each of prostate, bladder
and kidney cancer and the impact of financial toxicity, starting with
prostate cancer. A study from 2010 assessed out-of-pocket costs among
512 patients newly diagnosed with prostate cancer and undergoing either
radical prostatectomy or radiation therapy.
10 Participants
completed self-reported generic and prostate-specific HRQoL and
indirect-cost surveys at baseline and at 3, 6, 12, and 24 months
follow-up. Total mean out-of-pocket costs varied between radical
prostatectomy and EBRT groups at 3-month ($5576 vs. $2010), 6-month
($1776 vs. $2133), 12-month ($757 vs. $774), and at 24-month follow-up
($458 vs. $871). Linear mixed models indicated that radical
prostatectomy was associated with lower medication costs (OR 0.61, CI
0.48-0.89) and total out-of-pocket costs (OR 0.71, CI 0.64-0.92).
Prostate-specific HRQoL items of urinary function (OR 0.72; adjusted-CI =
0.58-0.84), bowel function (OR 0.96; adjusted-CI = 0.78-0.98), sexual
function (OR 0.85; adjusted-CI = 0.72-0.92), urinary bother (OR 0.79;
adjusted-CI = 0.67-0.83), and sexual bother (OR 0.88; adjusted-CI =
0.76-0.93) were inversely related to out-of-pocket costs. Surgical
approach may be a way to temper cost, as robotic prostatectomy has been
associated with a $138 decreased out of pocket cost to the patient
compared to open radical prostatectomy. Importantly, this is not a
problem among prostate cancer patients unique to the United States: both
Australia and Canada have reported financial toxicity among prostate
cancer patients.
Indeed, bladder cancer is an expensive disease to treat, with an
annual cost of nearly $4 billion per year, however little is known about
the financial toxicity among bladder cancer patients. As mentioned
earlier in the talk, the UNC study
5 showed that 24% of
patients endorsed financial toxicity (defined as “to pay more for
medical care than you can afford”). Participants who were younger (p =
0.02), black (p = 0.01), reported less than a college degree (p = 0.01)
and had noninvasive disease (p = 0.04) were more likely to
report financial toxicity. Beyond this one study, Dr. Penson notes that
there are no other studies assessing financial toxicity in this
expensive, complex, morbid disease.
According to Dr. Penson, kidney cancer financial toxicity is all
about the drugs. Over the past two decades, there has been an explosion
of new therapies for renal cell carcinoma. These drugs have inherently
changed the way we approach the disease and have resulted in benefit in
terms of prolonging survival. These agents, however, are quite costly
with annual wholesale costs of these agents ranging from $75,000 to
$200,000 per year. The risk of financial toxicity in this setting is
considerable and often not considered in medical decision making. While
other components in healthcare will contribute to financial toxicity,
Dr. Penson believes that the drugs are the key drivers here. A study
from 2015 assessed the associated costs for mRCC in the US using the
LifeLink Health Plan Claims Database.
11 A total of 1,527 mRCC
patients were analyzed; in 2010, nine unique treatment regimens were
used for first-line treatment, 8 for second-line treatment, and 8 for
third-line treatment. For 767 patients receiving modern therapy who were
< 65 years old, and stratifying by whether the first-line treatment
was oral or intravenous, drug cost per patient with ancillary services
was $59,664 versus $86,518, respectively (p = 0.001). Total costs and
drug out-of-pocket costs per patient during the first year increased by
the number of medication switches: $111,680 to $2355 for no switches,
$149,994 to $2538 for 1 switch, and $196,706 to $3524 for 2 or more
switches. Impressively, in 2004 the median drug cost was $11,458, while
by 2010 it rose to $68,660.
Dr. Penson concluded this talk on financial toxicity with the following summary points:
- Financial toxicity should be considered an adverse event of therapy, similar to other side effects of treatment
- This patient-centered endpoint can have a profound effect on our patient’s quality of life and daily existence
- While perhaps not completely avoidable, financial toxicity and its effect on our patients must be minimized
How can we help minimize financial toxicity?
- Discuss it upfront with our patients, creating an environment where
it is acceptable to talk about it. If you don’t know the specifics,
identify someone in your institution that dose
- Treat financial toxicity as another possible side effect when undertaking shared-decision making
- Think about the financial impact on the patient before you – do not
order discretionary testing or follow-ups that may not change
management, and do not initiate therapies that may have little or no
proven clinical benefit to the patient
- Consider the cost to the patient when choosing medical therapy for GU cancers
Presented by: David Penson, MD, MPH, Vanderbilt University, Nashville, Tennessee
Written By: Zachary Klaassen, MD, MSc – Assistant Professor of
Urology, Georgia Cancer Center, Augusta University/Medical College of
Georgia @zklaassen_md
at the 2020 Genitourinary Cancers Symposium, ASCO GU #GU20, February 13-15, 2020, San Francisco, California
References:
1. Ubel PA, Abernethy AP, Zafar SY. Full disclosure—out-of-pocket
costs as side effects. N Engl J Med 2013 Oct 17;369(16):1484-1486.
2. Zafar SY, Peppercorn JM, Schrag D, et al. The financial toxicity of
cancer treatment: A pilot study assessing out-of-pocket expenses and the
insured cancer patient’s experience. Oncologist 2013;18(4):381-390.
3. Narang AK, Nicholas LH. Out-of-pocket Spending and Financial Burden
Among Medicare Beneficiaries with Cancer. JAMA Oncol 2017 Jun
1;3(6):757-765.
4. Dusetzina SB, Keating NL. Mind the Gap: Why closing the Doughnut Hole
is Insufficient for Increasing Medicare Beneficiary Access to Oral
Chemotherapy. J Clin Oncol 2016 Feb 1;34(4):375-380.
5. Casilla-Lennon MM, Choi SK, Deal AM, et al. Financial toxicity among
patients with bladder cancer: Reasons for Delay in Care and Effect on
Quality of Life. J Urol 2018 May;199(5):1166-1173.
6. Gilligan AM, Alberts DS, Roe DJ, et al. Death or Debt? National
Estimates of Financial Toxicity in Persons with Newly-Diagnosed Cancer.
Am J Med 2018 Oct;131(10):1187-1199.
7. Kale HP, Carroll NV. Self-reported financial burden of cancer care
and its effect on physical and mental health-related quality of life
among US cancer survivors. Cancer 2016 Apr 15;122(8):283-289.
8.
Ramsey
SD, Bansal A, Fedorenko CR, et al. Financial Insolvency as a Risk
Factor for Early Mortality Among Patients with Cancer. J Clin Oncol 2016
Mar 20;34(9): 980-986.
9. Greenup RA, Rushing CN, Fish LJ, et al. Perspectives on the costs of
cancer care: A Survey of the American Society of Breast Surgeons. Ann
Surg Oncol 2019 Oct;26(10):3141-3151.
10. Jayadevappa R, Schwartz JS, Chhatre S, et al. The burden of
out-of-pocket and indirect costs of prostate cancer. Prostate 2010
Aug;70(11):1255-1264.
11.
Geynisman
DM, Hu JC, Liu L, et al. Treatment patterns and costs for metastatic
renal cell carcinoma patients with private insurance. Clin Genitourin
Cancer 2015 Apr;13(2):e93-100.
https://www.urotoday.com/conference-highlights/asco-gu-2020/asco-gu-2020-bladder-cancer/119188-asco-gu-2020-financial-toxicity-and-quality-of-life-understanding-and-improving-patient-centered-outcomes-in-genitourinary-malignancies.html