Pfizer Inc. (NYSE: PFE) will manage distribution of its COVID-19 vaccine on its own rather than through the U.S. government’s designated coordinator, but officials question whether the U.S. has an adequate supply of medical-grade freezers at the point of use for vaccines requiring storage at ultra-cold temperatures.
The Centers for Disease Control and Prevention in August tasked McKesson Corp. to be the central distributor for COVID vaccines and related supplies needed to administer vaccinations. Most pharmaceutical companies will deliver approved vaccines to McKesson distribution centers, which will arrange delivery to hospitals, nursing homes and other administration points.
Pfizer has a different, just-in-time distribution plan. It will ship COVID medicine directly from U.S. manufacturing facilities and warehouses to end users with the help of trusted transportation providers, said Tanya Alcorn, the company’s vice president for biopharma global supply chain, during a Thursday webinar organized by the U.S. Chamber of Commerce.
“We’ve been working from the beginning with the U.S. government to ensure that model is successful,” she said.
The U.S. government has contracted with the New York-based pharmaceutical company to deliver 100 million initial doses once its vaccine is approved, with an option for an additional 500 million doses. Pfizer’s product must be maintained at minus 75 degrees Celsius (-109.3 degrees Fahrenheit) to maintain its effectiveness. Officials this week said they expect to provide safety data from final-stage clinical trials to the Food and Drug Administration by the third week of November and then apply for an emergency use authorization if everything checks out.
Moderna also is also developing a vaccine for the government with similar technology and temperature requirements. It said Thursday it too is on pace to deliver data from a Phase 3 trial of its experimental COVID-19 vaccine in November. The company expects to be able to produce 20 million doses by the end of the year, and between 500 million and 1 billion in 2021.
Pharmaceutical and logistics industry representatives on the Chamber webinar said the U.S. is well positioned to handle ultra-cold vaccines, but federal health regulators last month expressed doubts about whether there is adequate infrastructure nationwide.
The responsibility for determining how many deep-freeze machines exist at health care facilities has fallen on states because there is no central inventory.
“Not all of those [vaccination sites] will have the ultra-cold deep freezers to be able to store vaccines, particularly the Pfizer product,” said Jay Butler, CDC deputy director for infectious diseases, during a mid-October media briefing. “So that is an important part of the state planning effort to determine where that capacity is.”
That means the nation’s 64 vaccinations jurisdictions are on their own to secure cryogenic freezers, which could lead to shortages as every region competes for a limited resource, much like states fought each other for ventilators early in the pandemic, Roll Call recently reported.
“There’s no historical precedent for us maintaining vaccines on dry ice in the United States. That’s never happened,” testified Paul Offit, an adviser to the FDA on vaccines and director of vaccine education at the Children’s Hospital of Philadelphia, before a House panel Sept. 30. “We’ve always shipped in the United States at most at freezer temperatures. … I do worry about that. I think it’s going to be an enormous challenge.”
Those worries are one reason some believe the Defense Department will deploy roll-on/roll-off cargo aircraft that can quickly transport large amounts of frozen vaccine, possibly in truck trailers, during the initial wave of distribution.
Experts say vaccines will likely be administered at hospitals and other large sites because typical spots such as pharmacies and doctor’s offices don’t have ultra-cold freezers. Large sites could share some of their shipments with local facilities if they have excess doses, but the vaccines could lose a day or two of freshness for transport, experts told Roll Call.
Nancy Messonnier, the CDC’s director of immunization and respiratory diseases, recommended during an industry conference call in late September against states investing in their own deep freezers, which cost as much as $15,000, because they won’t be needed for very long as less sensitive vaccines that take longer to develop are produced, according to the Roll Call report.
If sites quickly use up the doses ultra-cold storage may be less of a concern.
Medicines at standard frozen and refrigerated temperatures are much easier to distribute, according to industry representatives. Johnson & Johnson’s vaccine can remain stable at minus 20 Celsius.
“Our vaccine candidate is better suited to the world,” especially areas that don’t have the latest cold storage technology, said Remo Colarusso, vice president of supply chain at Johnson & Johnson, during the U.S. Chamber event.
Pfizer packaging innovation
Direct shipping enables Pfizer to have greater control and real-time insights into the status of the frozen vials.
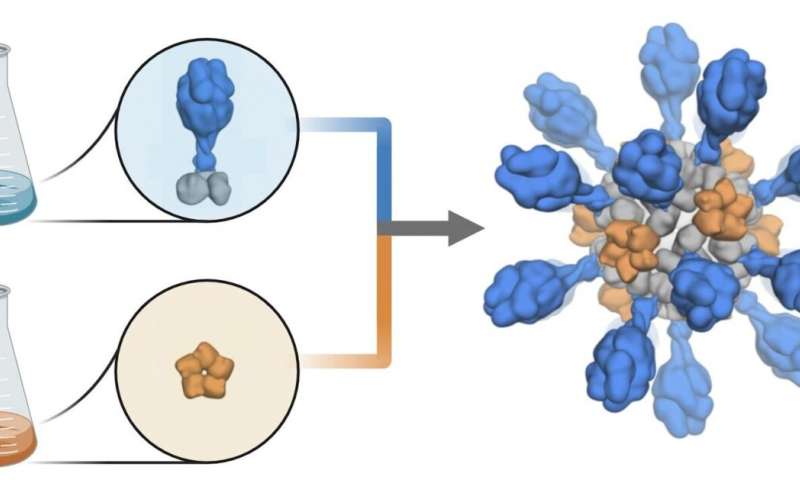
Uncertainty about the cold-chain capabilities of transportation providers and vaccine administration facilities led the drugmaker to co-create a special thermal cooler with real-time GPS and thermal monitoring that can keep its vaccine in a deep freeze for 10 days if left unopened. The shipping container, about the size of a small suitcase, uses dry ice to maintain recommended storage conditions. Once opened, vials can be stored at normal refrigerated temperatures for five days. Replenishing dry ice can extend the storage time after opening to 15 days.
Alcorn said Pfizer also developed a control tower that will get real-time alerts if the temperature deviates from the required range or a shipment doesn’t reach its destination within a prescribed time frame.
Control towers are centralized hubs with logistics specialists that capture data from all stages of the supply chain to improve processes and manage events.
Data loggers have provided GPS information for pharmaceutical shipments for several years, but Alcorn said having location data integrated with temperature readings from a refrigerated container is new for the industry.