by Susan Crabtree via RealClearPolitics.com,
The omicron variant may be nearing its peak in some states, but across the country it’s produced a dizzying array of conflicting signals on whether the nation should remain under a COVID national emergency or move on to an endemic “new normal.”
Omicron, for most people without co-morbidities, produces much milder symptoms than do the coronavirus’s previous variants, but it’s far more infectious, racing through schools, shutting down classrooms and forcing parents to consult their district’s ever-shifting COVID “decision trees” on a seemingly daily basis.
“When will the emergency end?” Justice Amy Coney Barrett, a mother of seven, asked during the Supreme Court’s recent vaccine mandate hearing.
It’s a question on most people’s minds.
As the country and the world enter the third year of the pandemic, many states have moved past the worst of the omicron outbreak, but in other parts of the U.S. the tally is still rising – fueling more questions about whether people are being hospitalized and dying with COVID or because of it.
There has been no consistent national reaction, leading to even more confusion about whether omicron is the beginning of the end of COVID or just another in an endless series of variants, each with its own dangers and, possibly, silver linings.
San Francisco last week announced that it will soon replace its indoor mask mandate with a kind of honor-rule system that allows added freedom if someone is fully vaccinated and boosted, although there’s no real verification system. On the other side of the country, however, New York state’s mask mandate is back in effect after an appeals court judge issued a stay on a lower court ruling that struck it down.
Meanwhile, some school boards in Virginia are in court fighting an executive order by new Republican Gov. Glenn Youngkin that allows parents to opt their children out of local school mask mandates.
After courts struck down the federal vaccine mandate for companies with more than 100 employees, President Biden subsequently rescinded the executive order. Now Starbucks, Boeing and Delta are rehiring employees fired for refusing to get the jab. Yet, other big companies are voluntarily keeping the requirement in place even as it hurts their businesses in the middle of a labor shortage.
In a particularly worrisome sign for the depleted health care field, nurses – who still must be vaccinated or face firing – are increasingly being allowed to stay on the job if they are COVID-positive but have mild symptoms or none at all.
As more people get COVID, there’s more natural immunity throughout the population, although just how much each variant provides is hard to know. Coronavirus antibodies generated by omicron infection last at least six months in 88% of cases, according to experts, but after that period the protection rate drops to 74%. Beyond that, it’s hard to predict.
It’s a disjointed patchwork of conflicting health policies and local responses, reflecting the lack of national consensus about just how disruptive the pathogen should still be.
While calls are intensifying to transition the country into treating COVID as an endemic disease – a state where its presence is constant but predictable and manageable – the Biden administration’s top experts warn it’s too soon.
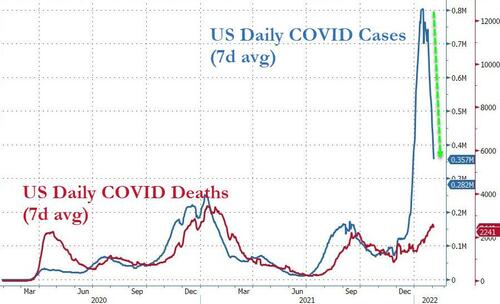
“When you have over 2,000 deaths, 150,000 hospitalizations, and you have people getting infected to the tune of somewhere around 700,000 a day, we’re not there yet,” Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, said last week.
Fauci, the national COVID icon reviled on the right while beloved on the left, then unveiled a worst-case scenario prediction for 2022: that there could be a new variant that evades vaccines and natural immunity. “I hope that’s not the case,” he said flatly.
Other health officials and political figures are striking a more hopeful note.
President Biden last week said the U.S. hasn’t yet reached its “new normal,” but added, “We’re moving toward a time when COVID-19 won’t disrupt our daily lives, when COVID-19 won’t be a crisis but something to protect against and treat.”
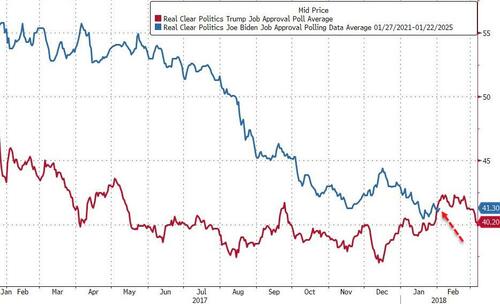
Cynical conservatives argue that Biden, whose flagging poll numbers are hurting Democratic prospects in November’s midterms, is shifting his rhetoric only in an attempt to convey a sense of control and calm ahead of those elections – even though omicron is still making that shift difficult if not impossible for many Americans.
When Biden took office, his plan to stop the virus relied heavily on increasing vaccinations, safely reopening schools, and pushing stimulus bills to help states and local officials battle the pandemic. But Biden and his top officials didn’t (and possibly couldn’t) anticipate omicron and the desperate need for testing that the rapid-spreader would spur. Critics and supporters alike argue the administration’s laser focus on vaccinations, including forcing people to get shots through mandates, came at the expense of producing and distributing more tests and therapeutics.
“They frankly focused on the vaccine – the vaccine did not end up being as extinguishing as we had hoped … and so they went ahead and added the booster,” Dr. Georges Benjamin, executive director of the American Public Health Association, told RealClearPolitics.
“In emergencies, the issue isn’t whether you made a decision that turns out not to be the ideal one; the issue is how you recover – and this administration has recovered well.”
But others argue just the opposite – that Biden waited far too long to pivot to more testing, and that the tests the administration is providing every American for free will only reach most people after the omicron peak has subsided.
“The Biden administration has failed its COVID test,” declares a recent headline in the Guardian, a left-leaning British newspaper.
In Europe, where the omicron surges have peaked ahead of the U.S., officials are more optimistic and appear more determined to move on and learn to live with COVID and any variants it spawns. The top European regional official at the World Health Organization recently that “omicron offers plausible hope for stabilization and normalization.”
British Prime Minister Boris Johnson a week ago announced an easing of coronavirus restrictions in England amid growing calls from inside and outside of his party for him to resign over his repeated violation of the rules.
Denmark, meanwhile, has announced plans to scrap all of its coronavirus restrictions and reclassify COVID-19 as a disease that no longer poses a threat to society despite infections remaining at record-high levels.
In the next month, Biden must decide whether to extend the national emergency status, which expires at the end of February. It’s a big decision with both practical and symbolic consequences. The emergency declaration, coupled with the public health emergency pronouncement issued by the Department of Health & Human Services, gives the federal government several critical tools to remove legal barriers and regulatory red tape, including the manufacturing of personal protective equipment by sources not yet completely reviewed by the Food and Drug Administration. It also allows HHS to use funding and authority under the Defense Production Act to improve onshore and near-shore production of vital resources. Additionally, it gives Federal Emergency Management Agency the ability to dispense PPE from the strategic national stockpile.
When it comes to health care providers, the emergency declarations authorize a long list of waivers from federal requirements – including expanding the type of health care professionals who can offer telehealth services billable under Medicare and Medicaid. It also allows hospitals and long-term care facilities to screen patients at locations offsite to prevent the spread of COVID.
The American Hospital Association earlier this month called on the federal government to renew both emergencies to ensure continued support for heavily burdened hospitals.
“The emergency declarations have proven critical in equipping hospitals and health systems with the tools and resources necessary to manage the recent COVID-19 surges and ensure high-quality care in this unprecedented environment,” the AHA wrote. “In their absence, the challenges of the pandemic will be exponentially more difficult to overcome.”
In mid-January, HHS Secretary Xavier Becerra extended his department’s public health emergency, continuing the declaration for another 90 days. This is the eighth time it has been extended since Becerra’s predecessor, Alex Azar, first announced it in January 2020.
But the White House hasn’t said whether it will extend the broader national emergency. A White House aide initially said he would look into the matter but didn’t respond to several follow-up questions from RCP.
Benjamin suggested Biden could follow HHS’s lead and provide just a 90-day extension instead of the year-long one he issued last year.
In addition to its practical impact on health care across the country, Biden’s decision will inevitably be politicized. Critics are likely to characterize any move to extend the emergency as proof that Biden didn’t shut down the virus as promised during his 2020 campaign – and to remind voters that the number of deaths during the first year of his presidency were similar to or only slightly less than the first year of the pandemic under Trump, despite having the vaccine in place.
Critics seized on Biden’s comments to U.S. governors in early January that there is “no federal solution” to the disease. Afterward, White House Press Secretary Jen Psaki and others tried to explain that Biden meant the federal government cannot solve the pandemic alone without working in partnership with governors and leaders at the local level.
But that explanation only poured fuel on the fire. Bobby Jindal, the two-term former governor of Louisiana, penned an op-ed for the Washington Examiner arguing that the milder omicron strain should spur a transition to endemic status.
“Emergency order expiration dates are looming,” he wrote. “… Policymakers need to relinquish emergency powers at the end of the surge and plot a sustainable path forward.”
Jindal quoted Dr. Monica Gandhi, a University of California, San Francisco infectious disease expert, who months ago predicted that COVID-19 would become endemic, like the flu, always circulating with seasonal peaks. The transition should occur when disease severity decreased and the immunity from vaccines and prior infections increased, she reasoned.
“We are amid that transition,” Jindal argued in his op-ed.
Four front-line health care providers also with UCSF agree. Last week they sent an online petition to California Gov. Gavin Newsom, all public school superintendents, and every county public health officer in the state, calling for a pivot in language that recognizes the virus as an “endemic.” This pivot, they argued, should coincide with an end to remaining restrictions, “particularly as they apply to children.”
The change.org petition had more than 30,000 signatures by Sunday evening. “We are particularly concerned about the toll that our state policies continue to have on children and teens,” the doctors wrote. “We are writing to ask California officials to acknowledge the endemic nature of COVID-19 after the omicron surge and immediately shift our public dialogue toward defining a path for removing all remaining COVID-19 restrictions in public schools.”
In addition to promising to shut down COVID, the Biden administration pledged to let scientists and public health experts drive its pandemic strategy. But omicron has produced such differing opinions among health experts and scientists that it’s scrambled the plan to have consistent and authoritative public policies, according to some health experts.
Lindsay F. Wiley, a health law professor at UCLA, said recent missteps by the CDC have once again damaged public trust and reinforced public perception that the administration’s guidance is “pretty chaotic.”
“There’s confusion after the CDC changes its guidance, and [it] has not always provided a robust explanation or justification for that change,” she told RCP, noting the back-and-forth on mask guidance and more recent changes governing isolation and quarantine that at first did not incorporate any kind of testing.
But, “the national emergency [declaration] is a much different framework than most people assume,” Wiley added, “so [it’s] still playing an important role and is still an appropriate measure in my opinion.”
Benjamin agreed, although he recommends Biden extend it for only a few months at a time, instead of continuing the declaration for a full year. Potential new variants are developing, and though Benjamin said they thus far don’t seem too worrisome, he warned of unpredictable twists and turns ahead.
He described three possible future COVID scenarios. The worst-case one, as Fauci outlined, would involve the development of an extremely infectious and lethal variant similar to delta. Another possibility is more seasonal outbreaks of COVID, as with the flu. And the third, he said, are spats of reoccurring lethal outbreaks in different states, which would require resources being moved around to put those fires out.
“We're still tracking other new variants that are developing day by day,” he said. “We don't think that there are problems, but this is going to be an issue for a while.”
https://www.zerohedge.com/political/covid-still-national-emergency-biden-must-soon-decide