by Roger Simon
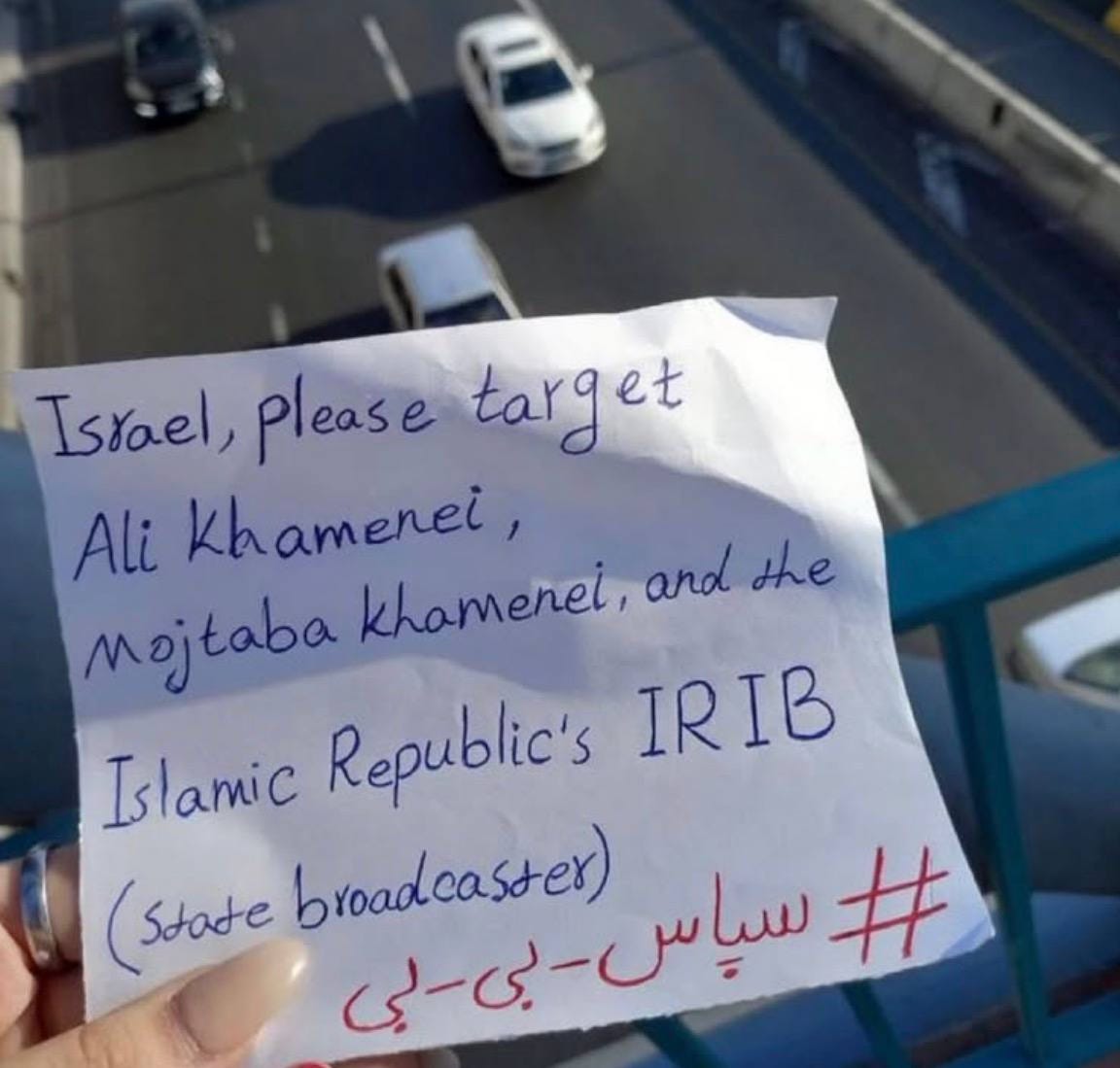
(“From a bridge in Tehran, an Iranian woman asks Israel to eliminate Iran’s supreme leader and his son in addition to attacking the IRIB television and radio network.” — Amir Tsarfati)
While some debate whether regime change in Iran is ongoing, it is already happening.
And of course it is necessary. As one of the now deceased Iran nuclear scientists explained just weeks ago, their scientists and nuclear installations can all be destroyed but the information required to construct weapons remains. Everything can be reconstructed. True that.
But that’s just one reason regime change is mandatory. The other is what these sadistic Shiites do to women. The misogyny of the ayatollahs is beyond comprehension. This is regime that got started by scraping makeup from women’s faces with razor blades. It got worse from there, especially regarding females who were incarcerated, almost always falsely..
Here’s just a tinge from Grok since it’s been my observation that most Americans, even supposedly educated ones, don’t know much about this:
“… there is substantial evidence from multiple sources, including human rights organizations, former prisoners, and international reports, indicating that the Iranian regime has engaged in the systematic rape of female prisoners, particularly virgins, before their executions. This practice, rooted in a distorted interpretation of Islamic law, was especially prevalent during the 1980s, notably during the mass executions of political prisoners in 1988. The justification was based on a belief that virgins would go to heaven if executed, and rape was used to prevent this. These acts were often framed as "forced marriages" or "temporary marriages" (sigheh) to prison guards or officials, ensuring the women were no longer virgins before execution.”
While doing research for the screenplay “Keys to Paradise” that is set in Iran, Sheryl and I learned that the parents of the raped women were informed of this “marriage” of their daughters that very night as a final exercise in what one might term paleo-sadism.
At that time we also met several of the former political prisoners whose faces resembled Picasso’s from the artist’s cubist period, their bones beaten into distortion from repeated beatings. Your heart went out to them even as you had difficulty looking directly at them.
To put it mildly, this made me partial to regime change. Horrifying as it is, I could not but approve when I saw this video Jun16 from Iranian TV that is a harbinger of the change that is coming rapidly. (Watch to end)
These evil people could have met their end years ago were in not for Barack Obama. Here’ another excerpt from Grok about what I consider close top the darkest moment of US, when we betrayed freedom to such an extent many of us were sickened:
“The phrase ‘Obama, are you with us or are you with them?’ was reportedly chanted by Iranian demonstrators during the 2009 Green Movement protests, which erupted after the disputed presidential election on June 12, 2009. These protests, sparked by allegations of electoral fraud in favor of incumbent President Mahmoud Ahmadinejad, saw millions of Iranians, particularly supporters of opposition candidate Mir Hossein Mousavi, take to the streets. The specific chant emerged as a plea directed at U.S. President Barack Obama, reflecting some protesters' desire for international support, particularly from the United States, amid the Iranian government's violent crackdown.”
Obama was obviously “with them,” as he elected to “negotiate” (to no end, needless to say) with Ahmadinejad rather than support the demonstrators in any meaningful way.
Many have speculated on why Obama did that, so I won’t do so except to say that those who pretend to the monikers “liberal” and “progressive” are the furthest thing from those.
https://americanrefugees.substack.com/p/dont-stop-israel-regime-change-now