Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I'm Dr F. Perry Wilson of the Yale School of Medicine.
The most complicated subject in my med school training, hands down, was immunology. So complicated, so confusing, and so vital to our survival that I decided to do the rational thing and become a nephrologist.
One question that always stuck in my brain from those early days was pretty straightforward: Why do we get some diseases only once, like measles, and others over and over again? Why can we gain lifelong immunity after exposure to, say, smallpox, but not to influenza A?
Of course, the pandemic has changed that question a bit, to: Why can we get reinfected with the coronavirus?
I was inspired to look into this question when this research letter from JAMA Pediatrics came across my desk. It's, fundamentally, a study about coronavirus antibodies, but it is special due to three factors.
First, it examines neutralizing antibody titers, telling us not only that antibodies are there, but that they can inhibit the ability of the virus to bind. Second, it looks at those levels over time in the same individual, so we can watch them rise or fall after an infection. And third, the study participants were all children. It gives us the best window yet into what is happening, immunologically, to kids who have had COVID infection.
In Singapore, 126 kids took part in the study. They all had neutralizing antibody levels measured within 1 month after a coronavirus infection. None of these kids had yet been vaccinated. The authors then did their best to follow the kids over time, measuring antibody levels at 1-3 months, 9-13 months, and 14-16 months later.
The findings are generally encouraging. Neutralizing antibody titers were high and actually increased a bit in the first 3 months after a COVID infection. Levels declined after that, but not dramatically. By 14-16 months, the median kid still had antibody levels that were sufficient to inhibit more than 50% of spike protein binding. The authors note that this is significantly longer protection than has been seen in adults.
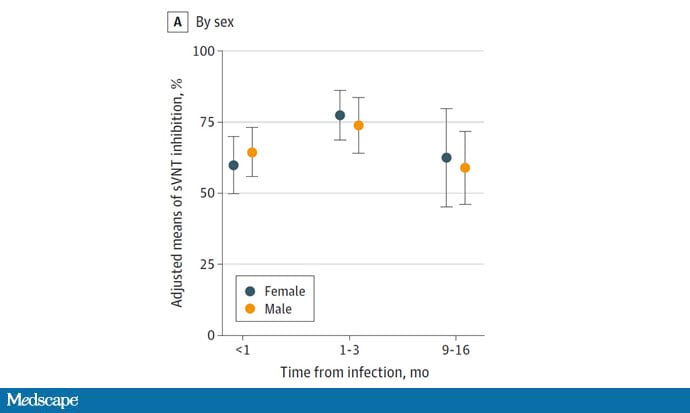
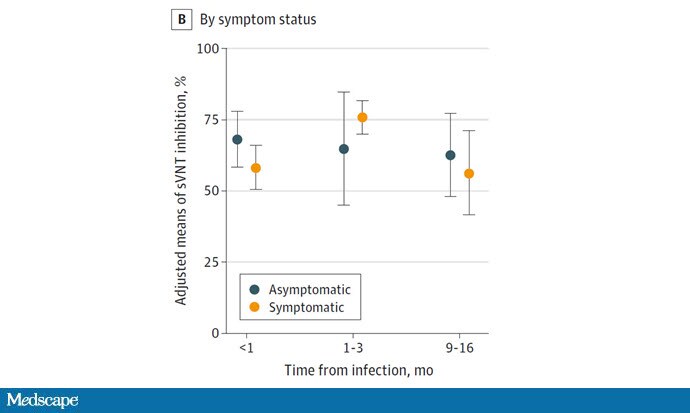
You can see that there was really no difference between boys and girls, or even among those with or without symptomatic infection.
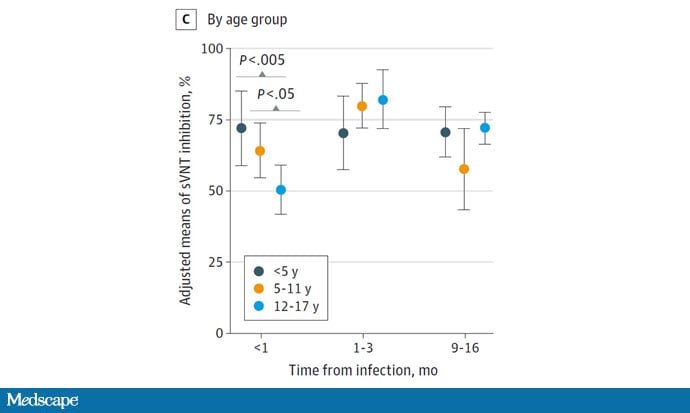
While older kids mounted less of an initial neutralizing antibody response than younger kids, levels quickly achieved parity.
Let's put this study into a broader context. After the Omicron wave, there are vanishingly few kids who have no immunologic record of SARS-CoV-2, either through vaccination or, increasingly, infection. This study would suggest that neutralizing antibodies persist at least for a year in kids, which has significant implications for when booster vaccines might be recommended relative to prior infection. It also suggests that reinfection rates may be lower in kids than adults, though reinfection rates in kids are hard to capture as they tend to be so mild.
Maybe, for kids at least, SARS-CoV-2 will act more like prevaccine measles than flu — a one-time infection that provides long-term protection. It does not seem to behave that way in adults. And to be honest, I'm not sure why.
There are a few reasons, according to infectious disease researchers, that some diseases are one-and-done and some lead to reinfection.
This New England Journal paper examined the long-term antibody responses to a host of one-and-done diseases, from smallpox to Epstein-Barr virus. You see antibodies lasting decades here in two example patients, including a spike after a smallpox booster vaccine.
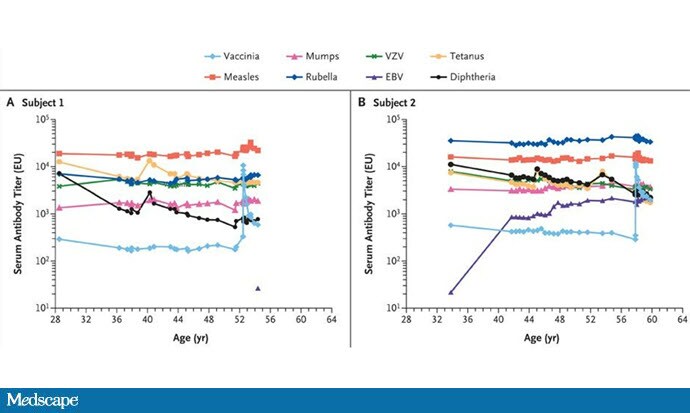
One common thread? These viruses don't mutate terribly quickly, making it more difficult for them to evade our immunity. And while SARS-CoV-2, on its own, doesn't have a mutation rate near that of the classically unstable influenza A virus, the sheer number of pandemic infections has allowed for variants to emerge in a timescale orders of magnitude faster than what we might see when SARS-CoV-2 becomes endemic.
Of course, if you're a parent, you really only care about one thing: Will the kids be all right? This week's study provides some reassurance that their young immune systems seem quite well poised to recognize this novel pathogen and, more important, to remember it into the future.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale's Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com.
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.