Matthew F. Watto, MD: Welcome back to The Curbsiders. On tonight's episode, we are going to be talking about back pain. This is based on an interview, Back Pain Update with Dr Austin Baraki. He gave us some great pearls about how to manage back pain, which we see so much of in primary care. I'll use one of my famous teaching techniques: If the patient has any kind of back pain, they should just not move. Right?
Paul N. Williams, MD: That's right, Matt-we should recommend bedrest until they get better for anyone who has any back pain? No. For back pain, early activity and exercise are great. Patients are often concerned that physical therapy will make their pain worse, so they don't exercise. This misunderstanding is not surprising. They believe that if they are experiencing pain, it's facilitating more damage, which is not necessarily the case. It will get better, and a little bit of anticipatory guidance goes a long way in terms of managing patient expectations related to early mobilization, early exercise, and physical therapy.
Watto: Absolutely. One of the goals of treatment is symptom relief to the extent that we're able to achieve. We're not expecting the pain to go to zero. That just doesn't happen, especially if someone's on a medication long term. Another goal is return to function. We want them sleeping. We want them to be able to tolerate movement.
We have medications — NSAIDs and muscle relaxants, which are actually tranquilizers. But most therapy for back pain doesn't involve medications. It involves active movement, so we have to find movement that the patient enjoys doing. Passive treatments, things being done to patients, just don't work as well.
Williams: We should be clear — we're talking primarily about chronic back pain here. For acute back pain, we actually have some decent medications, but acute back pain tends to improve no matter what you do. We don't have much to offer pharmacologically for chronic low back pain. The best modalities usually involve physical activity of some kind.
Watto: Let's discuss the evaluation of back pain. Something that always comes up: Should we order imaging, and is there a right time to get it? Dr Baraki was very clear about when to do imaging. Two big buckets of patients might need imaging.
First, a patient who has a serious underlying condition and you're using imaging to try to diagnose it; or in a chronic setting, a patient who needs surgery, and imaging is part of the presurgical evaluation. We talked about red flags.
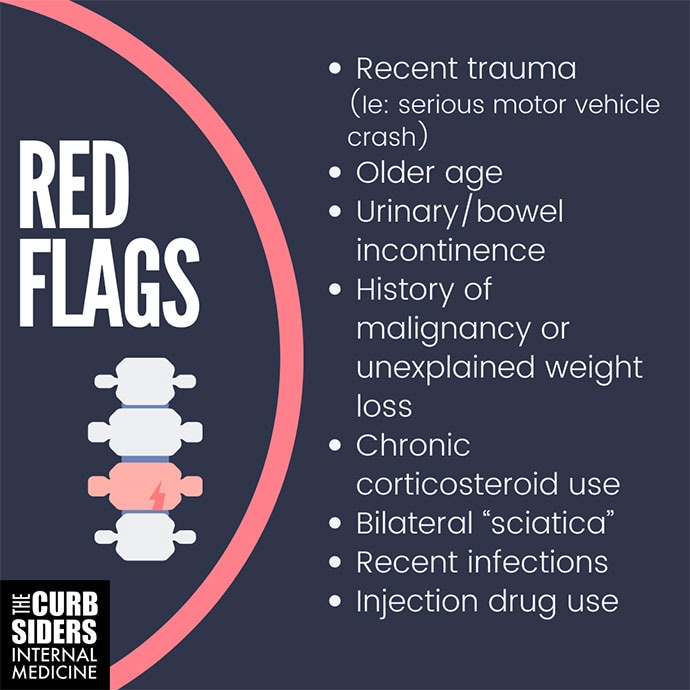
The red flags are major trauma, where we have reason to believe there might be something going on — if we strongly suspect infection, or the patient is injecting drugs. If the patient has a history of cancer, we would be worried that they might have a recurrence. Those are some of the main red flags. With a patient who has osteoporosis or is on chronic steroids, you might even be able to get by with plain films instead of an MRI to look for fracture.
The other thing I wanted to ask you about is, when should we get imaging? Are there any pitfalls we need to worry about?
Williams: I always like podcasts I'm not on because I enjoy listening to them much more. Dr Baraki talked about the very specific language that is used in radiology reports, such as spondylitis, spondylolysis, and multilevel degenerative disease. They sound bad, but if they are just reframed as age-related degenerative changes, that sounds so much more benign. When discussing with patients, we should avoid medical jargon and say that we saw some changes that we would expect for someone of your age. That sounds so much better than saying we saw multilevel degenerative disease, which sounds like an alarming pathology if you're not a physician. Without being inaccurate, we should frame the discussion such that we aren't providing a very specific diagnosis, because that is rarely the case with chronic low back pain. Typically, many things are going on and you may never identify a single unifying diagnosis, which doesn't tend to help anyway.
Watto: There's evidence showing that if the radiology report uses clinical terminology that both clinician and patient think of as less serious, they are less likely to proceed to more invasive treatments. Calling an episode of back pain a "lumbar strain" helps the patient understand that this is a pretty common thing. Almost everyone is going to have an episode of back pain at some point in their life, and almost all of them will get better. Most of the time there's no serious underlying condition.
This was a great discussion with Dr Baraki. Click on Back Pain Update with Dr Austin Baraki to hear the full discussion. Until next time, I've been Dr Matthew Frank Watto.
Williams: And I'm Dr Paul Nelson Williams.
Matthew F. Watto, MD
Clinical Assistant Professor, Department of Medicine, Perelman School of Medicine at University of Pennsylvania; Internist, Department of Medicine, Hospital Medicine Section, Pennsylvania Hospital, Philadelphia, Pennsylvania
Disclosure: Matthew F. Watto, MD, has disclosed no relevant financial relationships.
Paul N. Williams, MD
Associate Professor of Clinical Medicine, Department of General Internal Medicine, Lewis Katz School of Medicine; Staff Physician, Department of General Internal Medicine, Temple Internal Medicine Associates, Philadelphia, Pennsylvania
Disclosure: Paul N. Williams, MD, has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: The Curbsiders Received income in an amount equal to or greater than $250 from: The Curbsiders
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.