by Marina Zhang via The Epoch Times (emphasis ours),
There was an unexpected surge in the diagnosis of Type 1 diabetes among children and teenagers worldwide amidst the global impact of the COVID-19 pandemic, according to a new study.
The systematic review, published by the Journal of the American Medical Association (JAMA), analyzed 42 studies on diabetes incidence, including 17 studies involving nearly 38,000 people under the age of 19. The review revealed a 14 percent surge in Type 1 diabetes cases in 2020, followed by a 27 percent increase in 2021, compared to before the pandemic.
Furthermore, the research highlighted a rise in Type 2 diabetes incidence and diabetic ketoacidosis, a severe complication of diabetes more common in Type 1 patients, after the start of the pandemic.
What Is the Link Between COVID and Type 1 Diabetes?
The exact connection between COVID-19 and the higher risk of developing diabetes is unclear, according to the authors of the study. However, some doctors disagree.
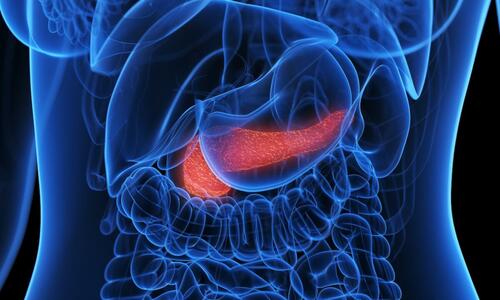
Type 1 diabetes is well established as an autoimmune disease, where the body attacks its own pancreatic beta cells, a primary source of insulin.
Both viral infections and vaccinations are known triggers for autoimmune diseases, and COVID-19 and its vaccine could be no exception, Dr. Paul Marik, a critical care physician, former tenured professor at Eastern Virginia Medical School, and co-founder of the Frontline COVID-19 Critical Care (FLCCC) Alliance, told The Epoch Times.
Numerous case reports have documented instances where patients developed Type 1 diabetes following either COVID-19 infection or COVID-19 vaccination.
The spike proteins present in the SARS-CoV-2 virus, as well as those produced by the body after vaccination, are very likely to be causing autoimmunity, according to Dr. Marik.
“There is few doubts that SARS-CoV-2 spike protein is the most likely trigger of Type 1 diabetes,” Dr. Flavio Cadegiani, an endocrinologist and researcher at Federal University of São Paulo in Brazil, told The Epoch Times via email.
The primary role of COVID-19 spike proteins is to attach to ACE-2 receptors on cell surfaces and enter the cells. Pancreatic beta cells, which have ACE-2 receptors, are vulnerable to infection and potential damage caused by spike protein entry.
Spike proteins also share similarities with human proteins, and their presence may lead the body to produce antibodies that not only target the spike protein but also attack human tissues, including the pancreas.
This phenomenon of molecular mimicry is seen in vaccine-injured patients, and those with long COVID, Dr. Marik said. Studies have found autoantibodies—antibodies that attack the body’s own tissues or cells—in both groups of patients.
Type 2 Diabetes: More Common and Complicated Consequence
The study may mistakenly conflate Type 1 and Type 2 diabetes as the same disease, hence the “no clear underlying mechanism” conclusion, board-certified internist Dr. Keith Berkowitz told The Epoch Times.
Type 2 diabetes, compared to Type 1, is more complex and metabolic, influenced by factors like obesity, processed food, heart disease, blood cholesterol, and hypertension.
Dr. Berkowitz said he has observed a unique blood glucose dysregulation pattern in his post-COVID and post-vaccine patients.
Patients with Type 2 diabetes typically have high blood sugar levels with high or low insulin levels as the beta cells become fatigued. However, Dr. Berkowitz said he observed that some of his patients had low blood sugar alongside high insulin levels, a condition he said he has never encountered before.
“Even my well-controlled diabetic patients are not faring well, especially those who have received both vaccinations and had COVID infections,” Dr. Berkowitz added.
Dr. Berkowitz uses intravenous fluids to address these conditions in Type 2 diabetics, restoring their water balance and blood sugar regulation. “When a diabetic goes to the hospital, the first thing they do is administer intravenous saline because insulin doesn’t work well in a severely dehydrated cell,” he said.
Treatment for Autoimmunity and Type 1 Diabetes
Autoimmunity is a condition where the body’s immune system mistakenly identifies its own cells, tissues, or organs as foreign invaders and attacks them. This can lead to various autoimmune diseases.
But the body may be brought back into balance.
1. Remove COVID-19 Spike Protein
The spike protein may contribute to autoimmune disease, prompting doctors to consider therapies that may remove these inflammatory proteins.
Research suggests that fasting can trigger autophagy, the process of clearing old, damaged, and foreign proteins.
Intermittent fasting and prolonged fasts, even for three days, may “reset” the immune system, potentially reducing autoimmune activity. Fasting, however, is not recommended for children or pregnant or breastfeeding women.
Other recommended therapies for spike protein removal include ivermectin, an antiparasitic drug, and N-acetylcysteine (NAC) supplementation.
2. Supplement With Vitamin D
Vitamin D insufficiency, a common deficiency among the U.S. population, has been linked to autoimmune disorders.
Research shows vitamin D supplementation reduces autoimmune disease risk by 22 percent. Infants given vitamin D also have lower Type 1 diabetes incidence, a 2001 study found.
Vitamin D reduces inflammation and provides infection protection. Some scientists propose it helps the immune system differentiate between self and non-self.
Dr. Cadegiani stated that one of his first therapies is to increase Type 1 diabetes patients’ vitamin D levels between the range of 60 to 90 ng/ml, which is around 6,000 to 9,000 IUs of dietary vitamin D per day.
Vitamin D is also linked to improved insulin sensitivity.
3. Reduce Sugar Intake
Sugar contributes to inflammation, and studies have found that those who consume high levels of sugar over extended periods are at a higher risk of developing autoimmune diseases.
In the case of patients with Type 1 diabetes, Dr. Cadegiani said that cutting glucose and carbohydrate consumption reduces insulin, and, therefore, can prevent the body from forming more autoantibodies against pancreatic beta cells.
4. Hydroxychloroquine
Dr. Cadegiani said that he sometimes prescribes hydroxychloroquine when a patient is positive for Type 1 diabetes antibodies, but still has around normal blood sugar levels.
The anti-malarial drug hydroxychloroquine is a powerful drug that fights autoimmune diseases. It is able to bind to the ACE-2 receptors and prevent spike protein entry and is also able to block spike protein from causing further harm.
It is currently approved by the U.S. Food and Drug Administration (FDA) for use in chronic discoid lupus erythematosus, systemic lupus erythematosus in adults, and rheumatoid arthritis, all autoimmune diseases.
Studies have shown that hydroxychloroquine can also reduce blood sugar and is associated with a reduced risk of Type 1 diabetes. The use of chloroquine, a hydroxychloroquine derivative, in Type 1 diabetes cases can reduce inflammation in the body.
5. Plant Supplements
Plant supplements like curcumin and berberine also have anti-diabetic properties and may help prevent Type 1 diabetes.
Curcumin can decrease blood sugar and insulin levels and reduce inflammation and oxidation. Some theories have suggested that curcumin may be able to prevent the immune system from overreacting, which results in autoimmunity.
Curcumin reduces inflammation in the gut, helping with digestion and overall gut health. An unhealthy gut can lead to a dysregulated immune system, increasing the risk of autoimmunity.
Despite being a plant compound, berberine has been found to have potent blood glucose-lowering properties. Berberine has been shown to be protective against pancreatic beta cells and also improve insulin resistance.
Thus, both patients with Type 1 or Type 2 diabetes may supplement with berberine. Those already taking medications for diabetes may need to consult their doctors before supplementing with berberine.
6. Diabetes Drugs
Dr. Cadegiani also uses diabetes drugs like metformin and liraglutide to treat and prevent Type 1 diabetes.
Metformin is a common diabetes drug that can reduce blood sugar levels. In Type 1 diabetes, metformin increases insulin sensitivity and action and also increases peripheral glucose uptake.
Liraglutide increases satiety and slows gastric emptying. Studies have also shown that the drug increases pancreatic beta cell mass, improves the cells’ functions, and prevents beta cell deaths, all of which may help prevent Type 1 diabetes.
https://www.zerohedge.com/medical/rise-type-1-diabetes-among-young-people-linked-covid-19
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.