by Eric Topol
Primary Prevention means a disease or condition is averted. The term was coined and introduced by Leavell and Clark in the late 1940s. Now, about 75 years later, we’ve yet to achieve any substantive primary prevention with the notable exception of vaccinations that prevent infectious diseases. Of the 3 major age-related diseases that I focused on in SUPER AGERS—cardiovascular, cancer, and neurodegenerative—we have not prevented the latter two. Remember screening for cancer (such as mammography, colonoscopy, PSA, or total body MRI as some have advocated without adequate data) is a secondary prevention, with the objective of finding cancer at an early stage. Nothing meaningful has yet been shown to prevent neurodegenerative diseases. While there has been some preemption of cardiovascular disease with the use of lipid panels and cholesterol lowering drugs, heart attacks (and heart disease) and strokes remain the number 1 and 3 medical causes of death in the United States, respectively. And heart disease deaths are ticking up, adjusted for age.
Instead our healthcare now is centered on treating these diseases, which has limited success for many cancers and even less, thus far no disease-modifying impact, for neurodegenerative diseases (Alzheimer’s and Parkinson’s). No less, there’s the profound economic benefit of primary prevention for reducing the cost of such treatments, such as tailored oncology drugs or support of people with dementia in long-term care facilities. I hope this brief review will convince you that primary prevention is a great and largely unfulfilled need, that in light of recent advances it should be given the highest priority. The key problem is that we haven’t had the ability to do it. Until now.
This Ground Truths post is about the new and exciting opportunity for achieving primary prevention. We’ll start with a groundbreaking study just published in Nature by Moritz Gerstung and his colleagues.
A Large Language of Health Model Predicting Individualized Risk for >1,000 Diseases — in Multiples and When
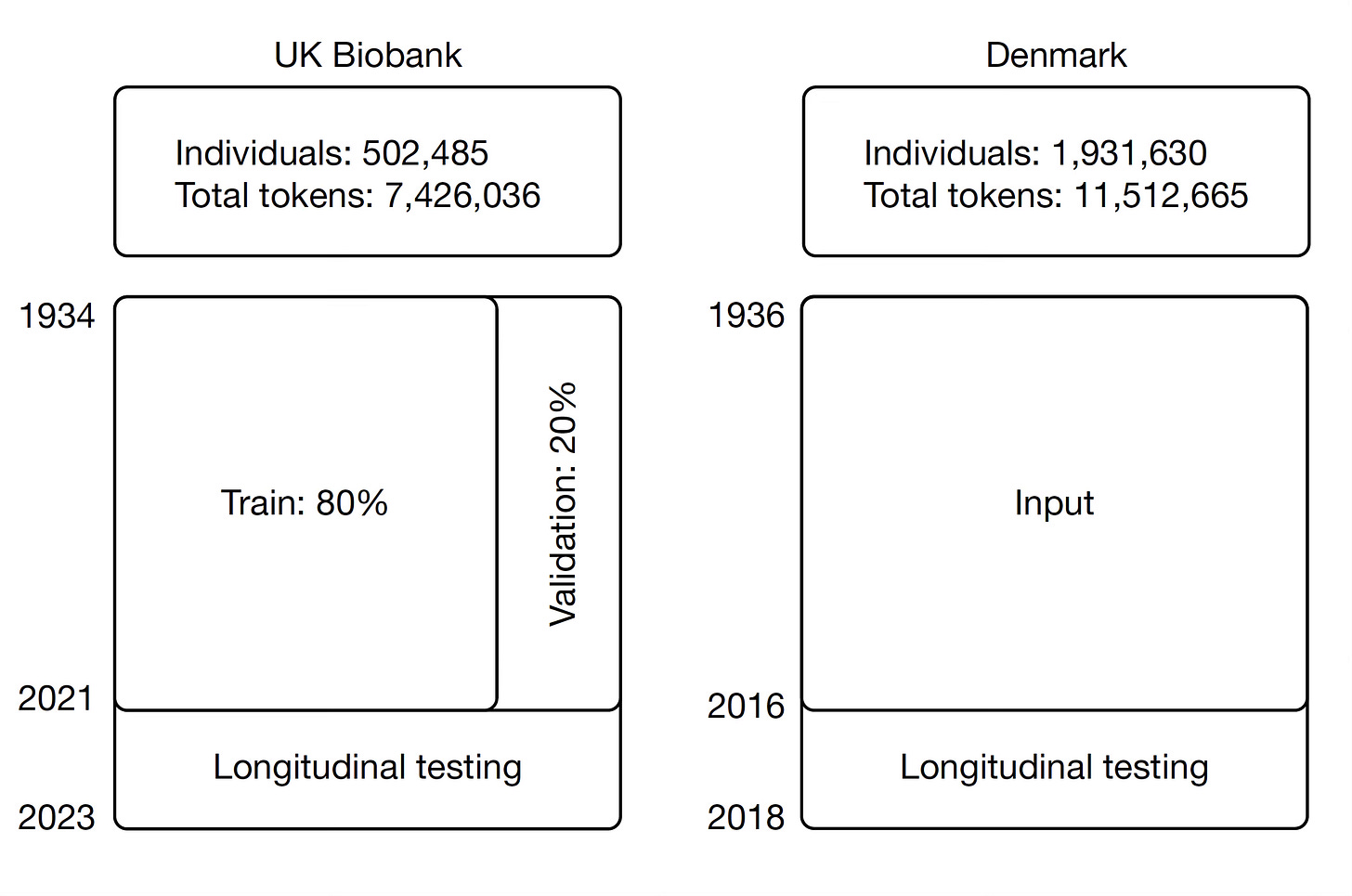
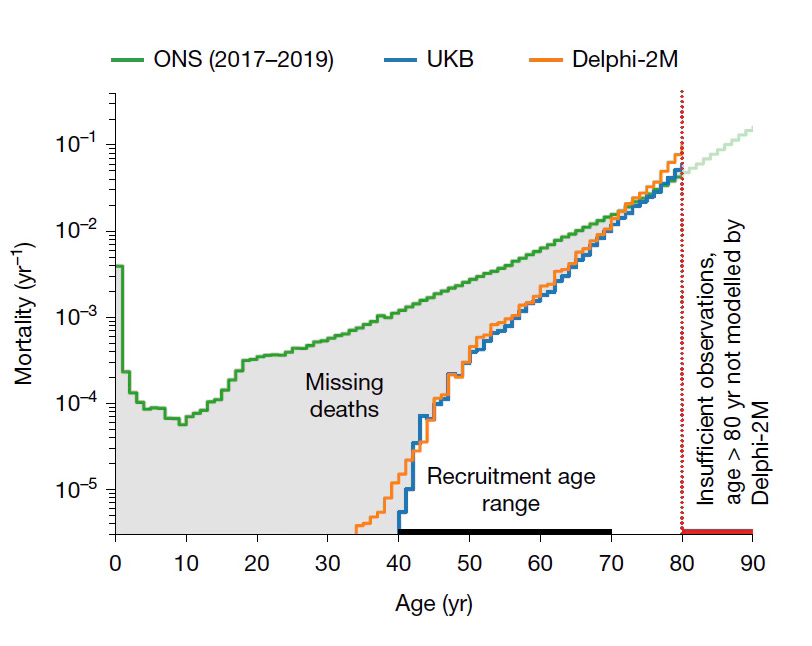
What if an individual’s arc of health events was like a sentence, a sequence whereby you could predict the next condition like you would with a transformer architecture A.I. autocompletion of words (hopefully a helluva lot better that we have now on our phones!)? That is the essence of generative A.I.’s power for text, using tokens of words (and word fragments) with extraordinary contextualization, giving it the ability to write high quality text, even books. Delphi-2M is a transformer, large language model (GPT-2 derived) learning the language of human health, that does exactly that but the tokens are based on diseases, sex, lifestyle and other related factors. It was built from the records, with long-term follow up, of 400,000 participants in the UK Biobank and externally validated in the Denmark population of 1.9 million people. Despite the participants in the UK Biobank being much younger, there was almost no difference in the Delphi-2M’s model performance for predicting diseases without any change in the parameters of the model. The input data included hospitalizations, primary care visits, self-reported information, and death registries.
Across >1,000 diseases, which is essentially the complete list of International Classification of Diseases (ICD-10), the Delphi-2M AUC (area under the curve, performance) was 0.76, and 0.70 over a 10-year span for prediction. The model was as good or slightly better than the best current single disease predictive models for dementia or heart disease (see below), and most others, but worse for Type 2 diabetes using HbA1c as single marker. Importantly, it predicted not just one but the multiple diseases (←when that risk was present) for an individual and the timing of appearance for each disease.
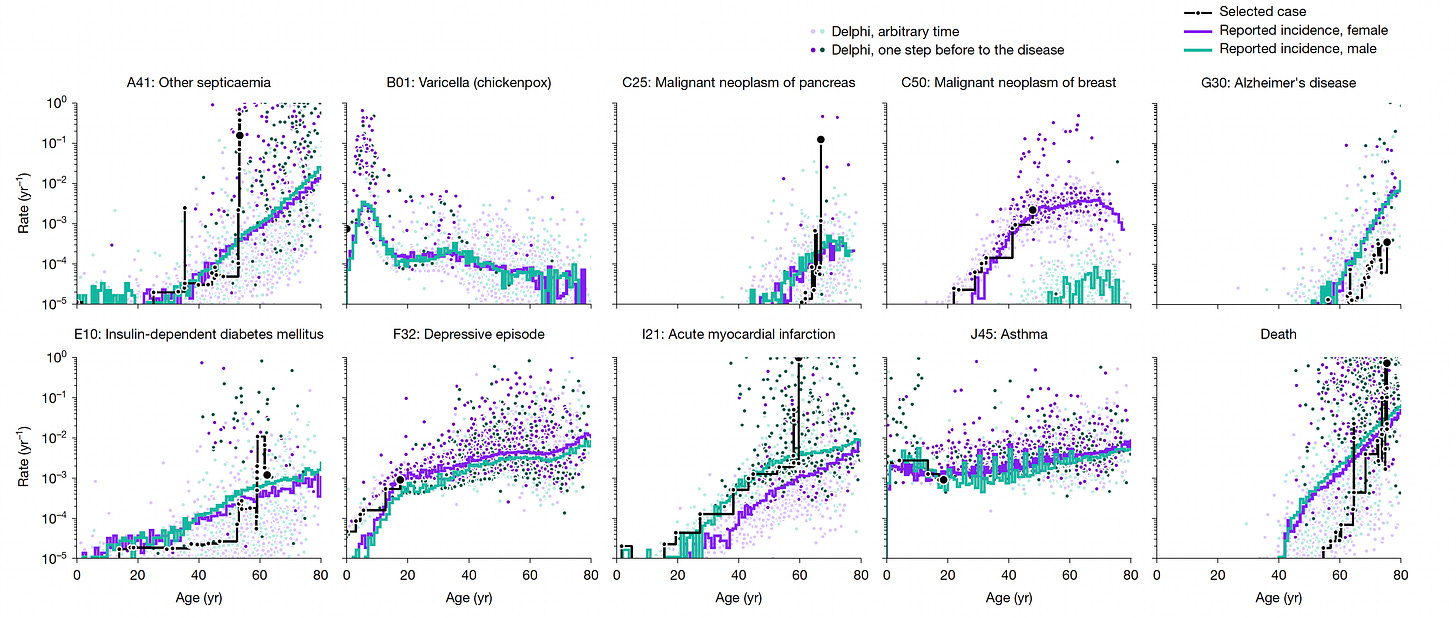
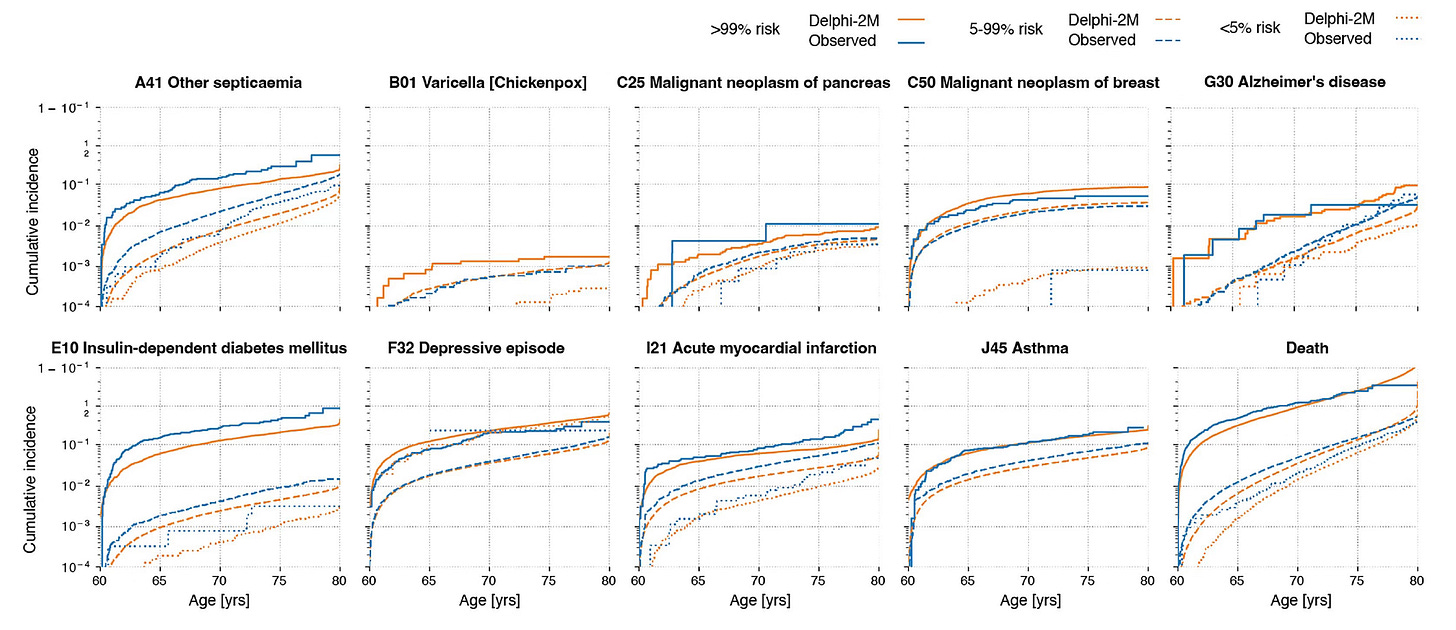
Below is the prediction of 10 diseases/conditions by the Delphi model and actual occurrence, specific to age.
For the outcome of death, the AUC was 0.97, age-stratified, for both sexes.
Using synthetic data to project a person’s future health from age 60 to 80, there was little reduction in the model’s performance (0.74 AUC).
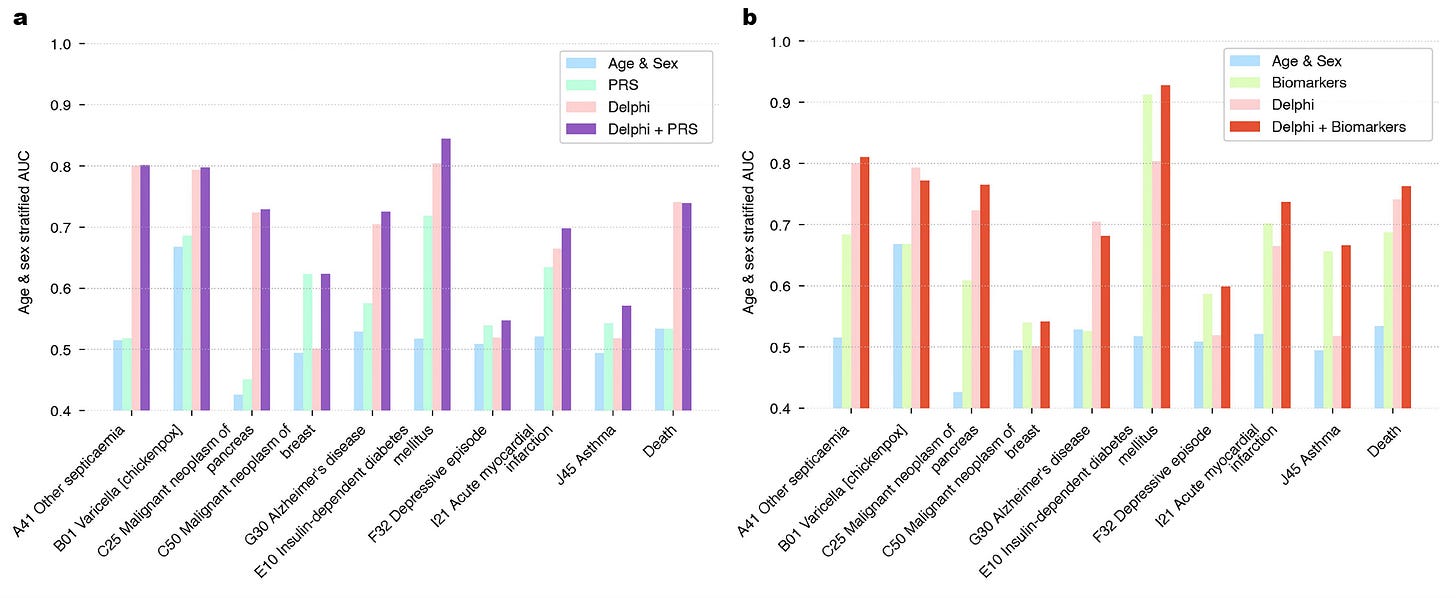
The model did not include many other layers of data such as polygenic risk score (PRS) or genome sequence, biomarkers, unstructured text from medical records, epigenetic or organ clocks, and several other potential layers that could be added. You can see how adding polygenic risk scores (at left below) or biomarkers (at right below) to the Delphi model took it even higher in accuracy for many diseases.
I won’t go into all the work put into their model explainability, with attention maps and ablation, but suffice it to say the success for predicting what disease(s) and when was tied, in part, to identifying patterns of clusters from the very large of sampling of people’s longitudinal health data.
Of course, there are many limitations to Delphi-2M, such as biases related to inputs of data. For example, people who were hospitalized had clusters of diagnoses attributed to being in a hospital, a type of data collection bias. There are ICD-10 disease token biases. And there were marked differences between healthy, younger volunteers in theUK Biobank vs sampling of the Danish population, but surprisingly little difference in model performance.
Other Related Major Advances
Here I’m going to highlight a few new papers that have come out in recent days and weeks that further bolster the case I made for primary prevention in SUPER AGERS. It’s inevitable—we’re going to age. But that doesn’t mean we have to manifest age-related diseases.
Personal Health Agent (PHA)
Instead of a single model like Delphi-2M that would be theoretically used chiefly by clinicians, Google DeepMind and Columbia University researchers published a multi-agent A.I. team approach that would process, interpret and be interactive with one’s personal electronic health record (including unstructured notes, labs, and reports) and wearable sensor data. Along with that the best sources of up-to-date medical knowledge. Employing a user-based design, from real world data from Google health queries, Fitbit forums, and surveys about personal health goals, a critical user journey was defined, divided into 4 areas:(1) general health knowledge; (2) personal data insights; (3) wellness advice; and (4) personal medical symptoms.
It’s a tall order because an analytic approach for doing this represents a formidable, previously unmet challenge. Just time-series analysis of multiple continuous data outputs from sensors had previously shown little progress. But with 3 A.I. specialized agents, one with expertise in data science, another a medical domain expert, and a third working as a health coach agent, the personal health agent performed exceptionally well according to benchmark ratings by human health experts (see the performance wheels below). The teamwork is coordinated by a project manager or orchestrator (bottom schematic) that harmonizes the work and output of the 3 agents across 4 steps. This is an important advance since we know lifestyle factors are critical for helping to prevent diseases, but we have not had a way to work with the multimodal data, get intelligence from it. Previously, we’ve basically been data collectors and have had limited interpretability restricted to one type of input (such as sleep data).
The PHA performed quite well. Compared with base model (Gemini), 65% of the summaries generated were found useful by clinicians compared with 30% of the base model.
Experts ranked the PHA as the best quality and most effective system for helping users achieve their goals in 80% of cases compared with 4% for a single-agent or 15% for a non-orchestrated multi-agent parallel system.
These are a sampling of evaluations of PHA, which, in general, was seen as more favorable for clinician reviewers than users, but both trending in the same direction. Of note, the PHA’s memory set up for long-term coaching and interaction, picking up where it left off, an essential feature for a PHA.
Again, there are many caveats and limitations including algorithmic bias due to inputs, security, the added consumption of computing power, data privacy, security, and over-reliance of the PHA by users. It clearly will require clinician oversight but can be seen as complementary to the Delphi-2M for directly helping patients. The most important limitation is that it has not yet undergone a prospective study in the real world of medicine compared to not having a PHA with the endpoint of pre-specified health outcomes.
Epigenetic Organ Age Clocks
I have written extensively about proteomic organ clocks and how they can give us considerable insight within an individual for accelerated pace of aging of our brain, heart, kidneys, liver, lungs, arteries and the immune system. A new report shows this can also be accomplished from methylation markers derived from a single blood sample using machine learning and A.I. integration with clinical biomarkers. Insights on aging for 11 organs or systems , as seen below, can be derived. Knowing that a person’s organ or immune system is out of step with the rest of their body for accelerated aging may be considered a tipoff to guide preventing a disease. For example, if the immune system has become senescent in a person, the risk of cancer will substantially increase. Recall we have not had any clinical way to assess the immune system until these clocks have arrived (and there’s more to come). The complementarity with proteomic clocks is a way to see if there is alignment, and both these tests will be inexpensive and likely commercially available soon.
Continuous Protein Monitoring (CPM)
Professor Shana Kelley and colleagues at Northwestern University published in Science an ingenious continuous, real-time sensor that used DNA strands to bind tightly to any protein circulating in the body, and electricity to get the protein off and assay it. Those of you who have tried continuous glucose monitoring (CGM) will know well how this works, applying the sensor just under the skin to sample interstitial fluid, then relaying your data to your smartphone. CPM was demonstrated in the diabetic rat model for tracking inflammation markers of interleukin-6 and tumor necrosis factor (Figure below, LPS is lipopolysaccharide). Last week I had a conversation on Ground Truths with Prof Kelly about this important discovery that has implications for prevention across many diseases (cardiovascular, autoimmune, neurodegenerative). She and her team have a review paper that will be published later this month that lays it all out and is outstanding.
The Template for Primary Prevention
As I presented in SUPER AGERS, we now have the means for defining high-risk individuals for the major age-related diseases. By using multimodal A.I. to integrate all the layers of a person’s data, we’ll be able to know whether a person is at high-risk and get an impression of the temporal arc of when a disease will appear (clinically manifest). Below is the example for cancer. We’ve already seen a number of studies demonstrating A.I. partitioning of high-risk and early detection of pancreatic cancer (among other cancer types) with much less depth of data than presented here. As you know, this is a highly fatal cancer which, in over 90% of cases, is only currently diagnosed at late, metastatic stages.
Alzheimer’s is the most dreaded disease for most people. Following a similar template as above for cancer (presented in SUPER AGERS), we will be starting a large randomized trial soon to prevent Alzheimer’s in people at high-risk due to their family history, APOE4 status, and polygenic risk score. Now that we have blood biomarkers that are modifiable like p-tau217, we’re in a powerful position to move forward.
Concluding Remarks
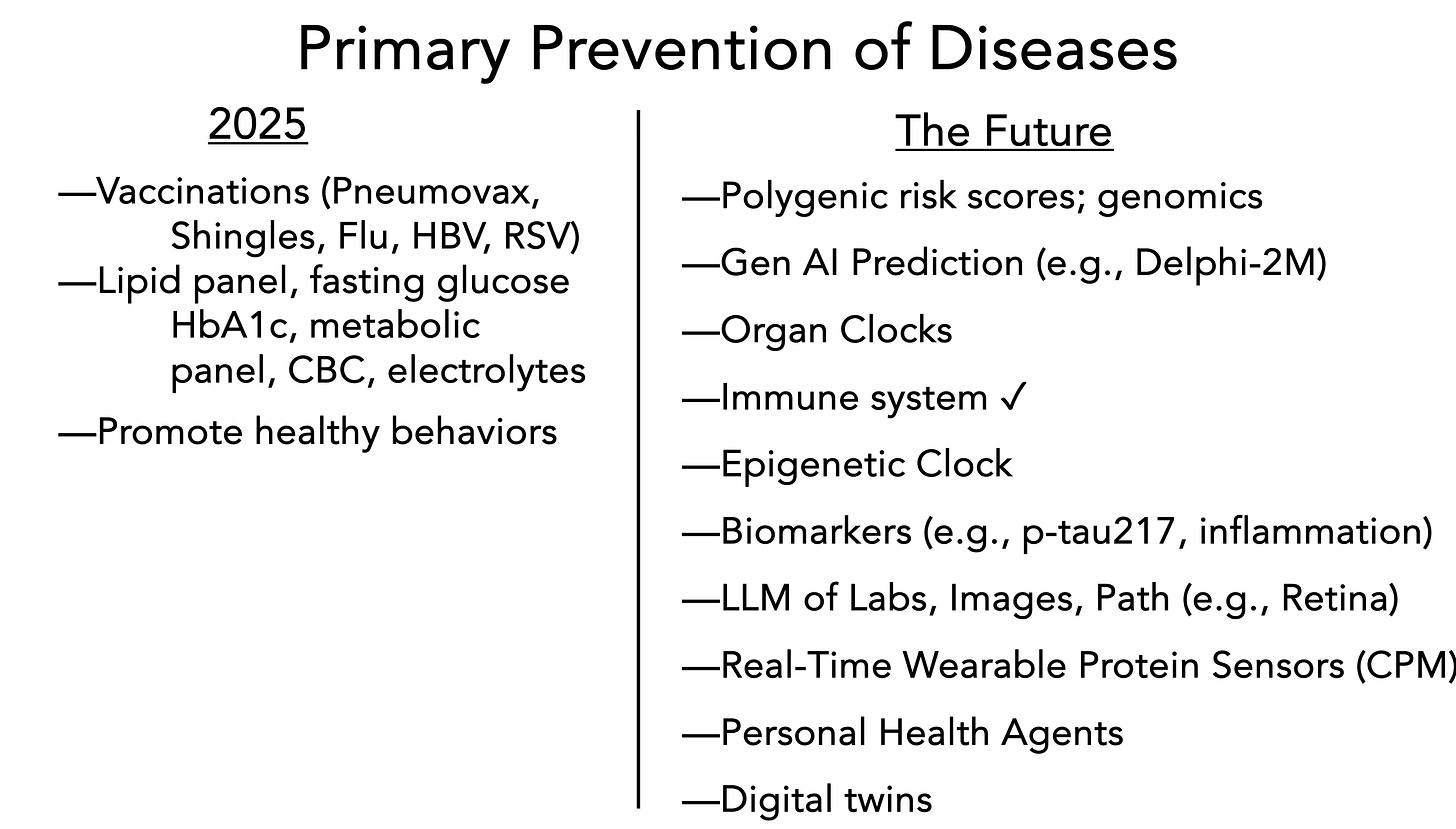
Here’s the contrast. At left below is state-of-the-art “primary prevention” today. Even that short list is not followed by a large proportion of primary care physicians or their patients. With the exception of preventing infectious diseases, it has little, certainly insufficient impact to prevent non-communicable, ,major age-related diseases.
At right, the future ,with many layers of new data that are already available (like p-tau217, polygenic risk scores, genomics). And many that will be available soon, such as organ clocks, an immune system clock and comprehensive assessment, A.I. of the retina, your images, and labs (trends in your “normal” lab values without an asterisk can be quite meaningful with A.I., as I previously reviewed). Eventually CPM and digital twin information resources (learning from nearest neighbor in our species) will be added to take primary prevention to an even higher level.
We’re at the dawn of primary prevention. Not only are there many new layers of data—organ clocks, biomarkers, genomics, biosensors—but we have multimodal A.I. and agentIc A.I. to analyze the data. For the first time, we are seeing a large health model (Delphi-2M) that has learned the grammar and language of health, tokenizing it to predict diseases with temporal anchoring. We’ve gotten used to large language models that predict the next word in a sentence, but just imagine how powerful a large health model (LHM) will be when all the other layers of data beyond those utilized in Delphi-2M are integrated. Yes, 0.76 AUC performance for prediction across all diseases isn’t great, but this is just the beginning. From Delphi-2M, we learned that person’s health story can be projected 20 years ahead. This represents a jump from my prior piece on precision medical forecasting. Future models will keep improving on precise medical forecasting.
At the same time, we’re seeing the most advanced personal health agent that has yet been developed and validated, which can incorporate layers of data not previously utilized, with interactivity and long-term memory that may help promote healthy lifestyles for users. No, it won’t work for everyone, but given poor adoption of healthy lifestyle factors (for example, 75% of Americans do not even fulfill the minimal recommendations for physical activity), it would be hard to think it won’t help to some extent.
There’s currently a lot of negativism about generative A.I. I get it. But the new era of primary prevention would not be possible without it. It will take time to get this to be standard of care, that is real prevention, but I believe it will ultimately wind up being seen as the most important contribution of A.I. for promoting human health.
https://erictopol.substack.com/p/dawn-of-a-new-era-of-primary-prevention








No comments:
Post a Comment
Note: Only a member of this blog may post a comment.