Although there is some slowdown as the U.S. Food and Drug Administration (FDA) moves into the holiday season in late November and into December, there are still upcoming target action dates. Here’s a look at this week’s PDUFA dates.
EyePoint Pharmaceuticals’ Durasert for Posterior Segment Uveitis
EyePoint Pharmaceuticals (formerly named pSivida), located in Watertown, Mass., has a target action date of November 5 for its New Drug Application (NDA) for Durasert for three-year treatment for posterior segment uveitis. Posterior segment uveitis is a chronic, non-infectious inflammatory illness that affects the posterior segment of the eye. It often also involves the retina and is a leading cause of blindness in the developed and developing countries. Current treatment is systemic steroids, but in time patients develop serious side effects.
“The FDA’s acceptance for review of our Durasert NDA submission is a major milestone for pSivida and we look forward to continuing to work with the FDA as they review our application,” said Nancy Lurker, EyePoint’s president and chief executive officer, in a March statement. “Given the high unmet medical need, we believe that Durasert, if approved, has the potential to become an important new treatment option for the thousands of patients suffering from posterior segment uveitis, the third leading cause of blindness.”
Durasert is a miniaturized, injectable, sustained-release drug delivery system that can last up to three years. It can be administered in the office setting via a needle as small as 25-gauge. So far, four products using the technology have received FDA approval: Yutiq (fluocinolone acetonide intravitreal implant); Iluvien (fluocinolone acetonide intravitreal implant), licensed to Alimera Sciences; Retisert (fluocinolone acetonide intravitral implant); and Vitrasert (ganciclovir), licensed to Bausch & Lomb.
Merck’s BLA for Keytruda in Advanced Hepatocellular Carcinoma
Merck & Company’s supplemental Biologics License Application (sBLA) for Keytruda for previously treated patients with advanced hepatocellular carcinoma (HCC) has a target action date of November 9. Keytruda is Merck’s dominant anti-PD-1 therapy. The application for this indication is based on data from the Phase II KEYNOTE-224 clinical trial, which was presented at the 2018 American Society of Clinical Oncology Annual Meeting in June and published in The Lancet Oncology.
“There continues to be a significant need for new options in the treatment of advanced hepatocellular carcinoma, which is the most common type of liver cancer,” said Scot Ebbinghaus, vice president, clinical research, Merck Research Laboratories, in a July statement. “The data supporting our application provide a clear rationale for the advancement of the Keytruda clinical program for hepatocellular carcinoma, and we are grateful for the opportunity to work with the FDA to potentially bring Keytruda to patients living with this difficult-to-treat cancer.”
On October 31, the FDA granted Merck’s Keytruda approval as a first-line treatment for patients with metastatic squamous non-small cell lung cancer (NSCLC). In fact, it seems as if the agency is approving Keytruda for something nearly every week. And if the FDA isn’t, the European Medicines Agency (EMA) probably is. The drug brought in more than $3.8 billion for the company in 2017.
Keytruda is a human programmed death receptor-1-blocking antibody. It is indicated for melanoma, non-small cell lung cancer, head and neck squamous cell carcinoma, classical Hodgkin lymphoma, urothelial carcinoma, microsatellite instability-high cancer, gastric cancer, cervical cancer, and primary mediastinal large B-cell lymphoma.
It was first approved for use in the U.S. on June 30, 2014.


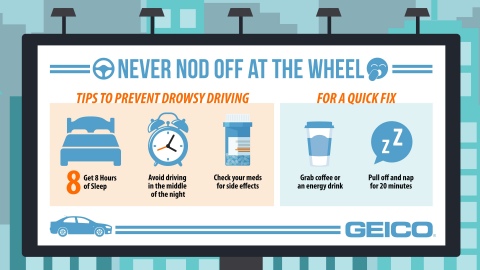 GEICO graphic with reminders about the dangers of driving while drowsy (Graphic: GEICO)
GEICO graphic with reminders about the dangers of driving while drowsy (Graphic: GEICO)