SY-1425 in Combination with Azacitidine Shows 63% Overall Response Rate and Rapid Onset of Clinical Responses in RARA or IRF8 Biomarker-Positive Newly Diagnosed Unfit AML Patients
Initial Data from Biomarker-Positive and -Negative Azacitidine Combination Cohorts Support Potential Predictive Value of RARA and IRF8 Biomarkers for Patient Selection
SY-1425 Induced CD38 Expression in Majority of Patients in Daratumumab Combination Cohort in Relapsed/Refractory AML and Higher-Risk MDS Patients
Both Combinations Have Been Generally Well-Tolerated to Date
Syros Pharmaceuticals (NASDAQ: SYRS), a leader in the development of medicines that control the expression of genes, today announced initial clinical data from cohorts in its ongoing Phase 2 trial evaluating SY-1425, its first-in-class selective retinoic acid receptor alpha (RARα) agonist, in combination with azacitidine and with daratumumab in genomically defined patients with acute myeloid leukemia (AML) and higher-risk myelodysplastic syndrome (MDS). These data are being presented at the 60th American Society of Hematology (ASH) Annual Meeting and Exposition.
“AML and MDS are complex diseases, and we need therapies that can be used in combination to help patients live longer and with a better quality of life,” said Rachel J. Cook, M.D., M.S., Assistant Professor of Medicine and Site Director for Acute Leukemia at the Knight Cancer Institute, Oregon Health and Science University and a clinical investigator in the Phase 2 study of SY-1425. “These data provide early clinical evidence that SY-1425 may be a meaningful treatment option for defined subsets of AML and MDS patients that is generally well-tolerated in combination with other therapies. I look forward to continuing to investigate SY-1425 to fully understand its potential to benefit patients.”
“These initial combination data from our ongoing Phase 2 trial of SY-1425 are promising,” said David A. Roth, M.D., Syros Chief Medical Officer. “SY-1425 in combination with azacitidine showed both a high response rate and rapid onset of clinical responses in AML patients selected with our RARA or IRF8 biomarkers that we have not seen to date in the biomarker-negative cohort. The combination was generally well-tolerated with no evidence of increased toxicities beyond what would be expected with each agent alone, including myelosuppression that can sometimes be seen when combining drugs to treat leukemia. These data speak to the combination potential of SY-1425 as well as to the potential of our platform to identify patients most likely to respond to gene control medicines. We look forward to further characterizing the clinical activity of SY-1425 in combination with azacitidine as we continue to enroll and follow patients in the trial.”
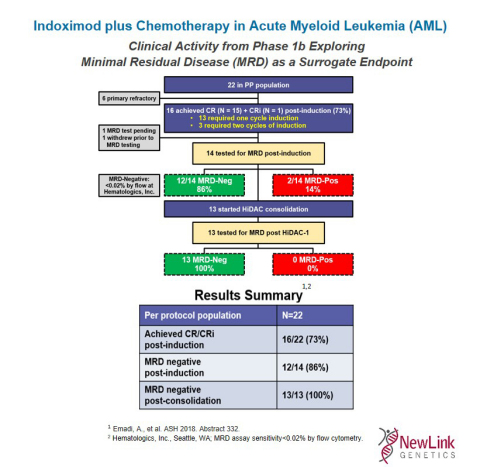 Indoximod plus Chemotherapy in Acute Myeloid Leukemia (AML) (Graphic: Business Wire)
Indoximod plus Chemotherapy in Acute Myeloid Leukemia (AML) (Graphic: Business Wire)