More than a year later, the Department of Health and Human Services (HHS) has rolled back a Trump-era policy that had limited the FDA’s oversight of lab-developed tests, or LDTs, which include a wide range of in vitro diagnostics which, although limited in scope, have grown in use over the past two decades.
LDTs are generally deemed low-risk products that are designed, produced and used within a single laboratory. But they can vary from simple, single-measurement blood tests to complex screeners for genetic mutations. They are employed in settings that scale from small hospitals up to the largest academic medical centers and health systems in the country as well as by certain companies that offer direct testing services.
They have not required the FDA’s clearance, approval or authorization compared to kits that are manufactured and distributed widely for use in independent labs. Yet, they have been steered by draft guidance documents and regulations over their components and the agency’s broader enforcement discretion.
But in August 2020, the Trump administration revoked what authority the FDA had established over LDTs, including requirements that certain COVID-19 tests go through the agency’s emergency review process.
At that time, HHS published a brief announcement saying that if the FDA wanted to challenge the policy, the regulatory agency would need to pursue a full, formal regulatory rule to reinstate any premarket review of LDTs. The Biden administration has now reversed that move.
“Effective today, HHS no longer has a policy on LDTs that is separate from FDA’s longstanding approach in this area,” HHS Secretary Xavier Becerra said Monday in an equally brief statement, adding that the previous approach had “limited FDA’s ability to address certain problematic COVID-19 tests.”
Meanwhile, members of the industry haven’t appreciated being caught in a regulatory tennis match: In a statement from the national trade group, American Clinical Laboratory Association (ACLA) President Julie Khani said, “Continually shifting regulatory policies creates uncertainty and undermines patient access to lifesaving diagnostics.
“This underscores the clear need for comprehensive diagnostic reform legislation that can provide long-term clarity and continuity for clinical labs and their work to support medical breakthroughs moving forward,” Khani added. The ACLA has previously lobbied HHS and the FDA to limit the agency’s authority to regulate LDTs as medical devices.
This week, the FDA also updated its policies for COVID-19 tests including coronavirus LDTs as well as rapid diagnostics for use in home and healthcare settings.
The agency said it plans to focus its review efforts on emergency authorization requests for mass-produced at-home and point-of-care tests, including for use with or without a prescription, in addition to certain lab-based, high-throughput diagnostics that can screen samples for multiple diseases at once.
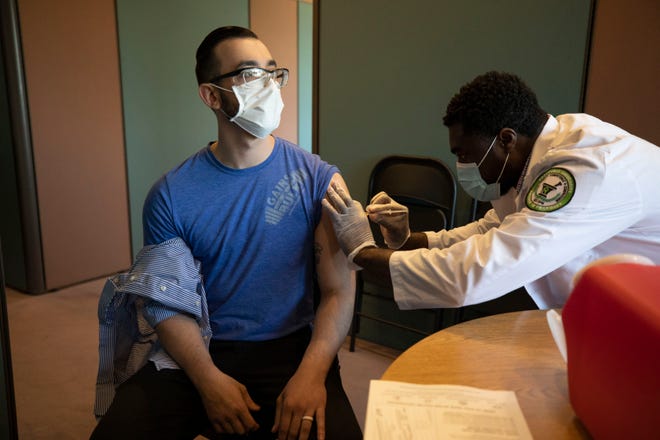
“In addition to vaccination efforts, testing remains a cornerstone of the national response to the pandemic and plays a central role in helping Americans get back to work, school and other important activities, particularly as the holiday season approaches,” the FDA’s device center director, Jeff Shuren, M.D., said in a statement.
“By focusing our review on these types of tests and helping to ensure that available tests have appropriate oversight, we can better respond to the pandemic as the nation’s testing needs to continue to evolve,” Shuren said.
The FDA also said it would prioritize certain antibody tests that can help quantitatively measure a person’s immunity to the coronavirus as well as diagnostics that are supported by the National Institutes of Health’s Rapid Acceleration of Diagnostics initiative or the Biomedical Advanced Research and Development Authority, better known as BARDA.
To date, the agency has granted emergency authorizations to over 420 tests and mail-in sample collection kits since the beginning of the pandemic. The FDA estimates its recent green lights for over-the-counter diagnostics could result in up to 400 million more tests per month on store shelves by early 2022.