Nektar Therapeutics (Nasdaq: NKTR) announced today that biomarker and clinical data from PIVOT-02 is being presented at the 2019 American Society of Clinical Oncology (ASCO) Meeting in Chicago, Illinois.
New baseline biomarker analyses and updated clinical study efficacy and safety results were shared in a presentation titled, “Baseline tumor-immune signatures associated with response to bempegaldesleukin (NKTR-214) and nivolumab” (Abstract #2623/Poster Board #267) by Michael Hurwitz, Ph.D., M.D. who serves as Assistant Professor of Medicine, Medical Oncology at Yale Cancer Center during the “Developmental Immunotherapy and Tumor Immunobiology” poster session on Saturday, June 1, 2019.
“The Stage IV melanoma patients enrolled in the ongoing PIVOT-02 study continue to experience both deepening and durability of response over time,” said Jonathan Zalevsky, Ph.D., Chief Scientific Officer at Nektar Therapeutics. “This translated into a 34% rate of complete response at a 12-month follow-up for the 38 efficacy-evaluable patients in this cohort. Further, 42% of patients achieved a 100% reduction in target lesions. Finally, corresponding lymphocyte data highlight the benefit of replenishing and stimulating T cells continuously over the course of treatment with an I-O doublet regimen.”
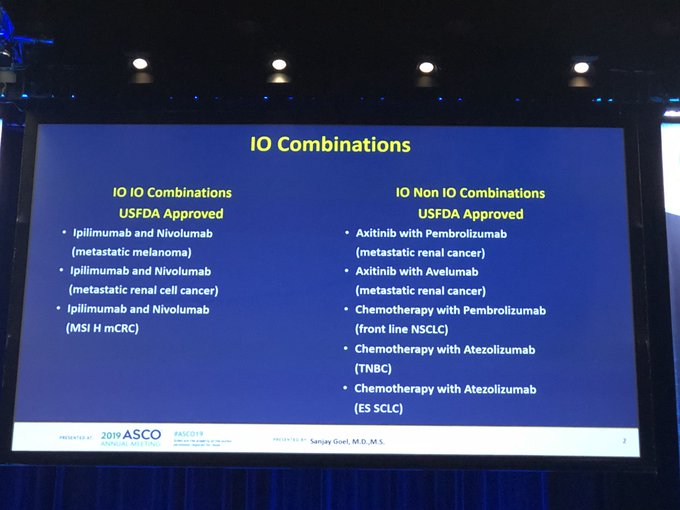
Bempegaldesleukin (NKTR-214, bempeg) is an investigational, CD122-preferential IL-2 pathway agonist designed to provide sustained signaling through the IL-2 beta-gamma receptor. PIVOT-02 is an ongoing Phase 2 study evaluating bempeg in combination with nivolumab in solid tumors.