The latest Travel Alert issued by the US Centers for Disease Control and Prevention (CDC) regarding Dengue outbreaks in the Americas may influence winter vaccination plans during 2020.
The CDC said in an updated Level 1 Travel Alert ‘dengue is an ongoing risk in many parts of Central and South America, Mexico, and the Caribbean.’
On December 23, 2019, this updated ‘Practice Usual Precaution’ Travel Alert said ‘the countries listed below are reporting higher-than-usual numbers of dengue cases, and travelers visiting these countries may be at increased risk:
- Belize
- Brazil
- Colombia
- Costa Rica
- Dominican Republic
- El Salvador
- Guatemala
- Honduras
- Mexico
- Nicaragua
- Paraguay
Dengue is common in more than 100 countries around the world, and about 3 billion people, live in areas with a risk of contracting 1 of dengue’s 4 virus types.
The CDC said ‘because dengue is spread by mosquito bites, all travelers to risk areas should prevent mosquito bites by using an EPA-registered insect repellent, wearing long-sleeved shirts and long pants when outdoors, and sleeping in an air-conditioned room or room with window screens or under an insecticide-treated bed net.’
There is no specific treatment for dengue, but early detection and access to proper medical care lowers fatality rates to below 1 percent, says the CDC.
In the USA, an infected mosquito (Ae. aegypti or Ae. albopictus) can spread the dengue virus to people through bites.
And, the CDC says a pregnant woman already infected with dengue can pass the virus to her fetus during pregnancy or around the time of birth.
Dengue disease can take up to 2 weeks to develop with illness generally lasting less than a week. The health effects from dengue include fever, headache, nausea, vomiting, rash, muscle and joint pain, and minor bleeding.
Dengue can become severe within a few hours. Severe Dengue is a medical emergency, usually requiring hospitalization. In severe cases, health effects can include hemorrhage, shock, organ failure, and death says the CDC.
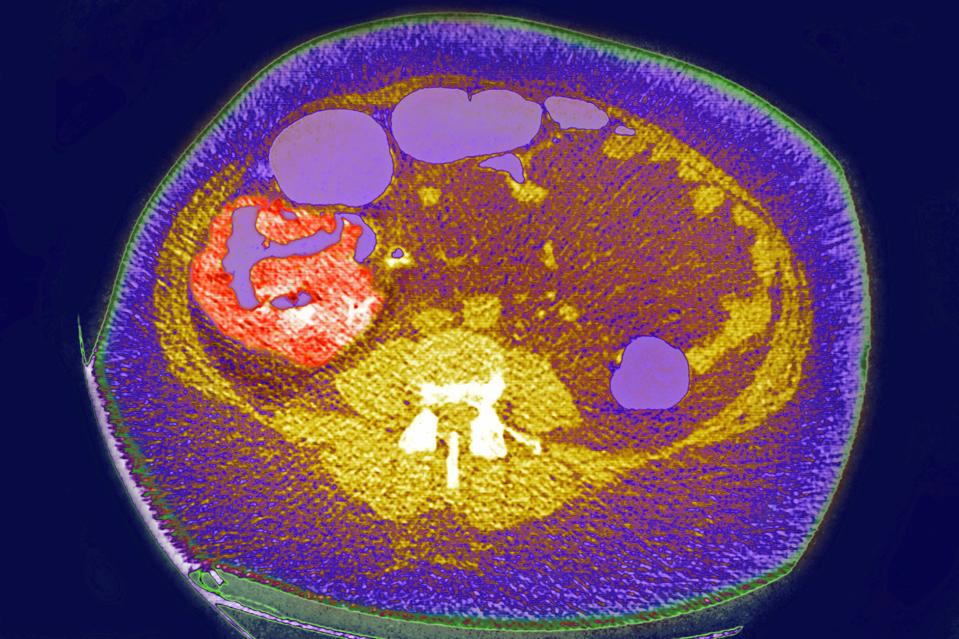
Regarding diagnosing a potential dengue patient, the CDC suggests healthcare providers should review the patient’s past medical history, recent travel history, travel notices regarding disease outbreaks, and vaccination record, especially for yellow fever and Japanese encephalitis vaccinations, to determine the likelihood that the patient’s recent illness is due to an infection with dengue virus.
On December 26, 2019, a new study reported the ‘screen and vaccinate’ strategy is more effective in reducing the number of hospitalized and Severe Dengue cases.
In the USA, the state of Florida has reported both travel-related and locally acquired Dengue cases in 2019.
On December 24th, 2019, the Florida Department of Health in Miami-Dade County (DOH-Miami-Dade) announced 2 new dengue cases of local transmission confirmed in Miami-Dade residents.
In total, Florida has confirmed 16 locally-transmitted dengue cases this year.
Previously, Florida’s Arbovirus Surveillance Week #51 report confirmed 391 travel-associated dengue cases in Florida, as of December 21, 2019. Miami-Dade County and Broward counties have reported the most travel-related dengue cases during 2019.
In total, the CDC confirmed 1,026 dengue cases in the USA, and an additional 46 in the US Territories, as of December 6, 2019.
Regarding preventive vaccines, Dengvaxia is the only approved dengue vaccine in the USA and in about 20 other countries. Dengvaxia is indicated for the prevention of dengue disease caused by dengue virus serotypes 1, 2, 3 and 4.
The CDC suggests people considering a dengue vaccination should speak with a qualified healthcare provider.