I had not even gotten to my morning tea today when this lurid headline crossed my path, courtesy of the Washington Post:
When I read the article, the plot grew even thicker; apparently, some are blaming the emergence of this super-bug on global warming. In fact, it is a “leading theory.” And, wait; did the Washington Post just use the words, “zombie apocolypse”??? Yes. Yes they did.
If these lines are not screaming, “Media Sensationalism,” to you, it is possible you need your hearing aids checked. I do not want to pretend that the emergence of a new strain of candidal yeast with some evidence for drug resistance is a good thing; it’s not. However, I want to reassure my readers who might now be terrified to set foot inside a hospital lest they be the next zombie victim of Candida auris. If you walked into the hospital of your own accord, the odds are overwhelming that you won’t be.
First, though, the usual caveats: I am not an infectious disease physician, and the last time I was regularly dealing with a new resistant fungus, it was the cousin of C. auris, Candida glabrata, and the year was 2005. However, the story line back then was not altogether dissimilar: considered a benign organism until the 1990s, we were now seeing a high rate of lethal infections with this fungus in very ill and immunocompromised patients. Making matters worse, C. glabrata generally was resistant to our usual anti-fungal medications, leading to a reliance on a then-new class of anti-fungals, the echinocandin drug class. Glabrata infections were serious business. I didn’t see a lot of headlines about them, however.
It’s 2023, however, so Candida auris is getting its day in the media sun. It’s new-ish, having been discovered in 2009 in a 70 year-old’s ear (hence the species name, “auris”), and even the staid NIH called it a “mysterious and tenacious enemy.” The most important part of the story, however, is the part that was left out of the article: candidal yeast is everywhere. Candida albicans is between most of our toes. Candida kefyr is in your tangy kefir drink. Even nasty Candida glabrata was found to colonize 25% of patients in a Detroit hospital in the early 1990s. The Washington Post article repeatedly refers to this threat simply as “Candida,” making statements like, “Authorities first detected Candida in the United States in 2016.” I can only imagine that their editor was sleeping in Monday morning; but it sure increases the risk of confusion from reading this bit of science news.
The Washington Post piece was inspired by Monday’s CDC “Immediate Release” on the subject, promoting their publication in the Annals of Internal Medicine. That someone would choose this Monday to rush out a breathless post on a pathogen being closely tracked for five years is beyond me; why not watch the Princeton-Arizona basketball game instead? The CDC continues to mystify me.
I can’t say the quality of their bulletin convinced me that their time had been well spent. (Having now watched the entirety of the Princeton-Arizona game twice, I suppose I could be similarly accused.) Yes, numbers of reported cases are rising, from 476 in 2019 to 1,471 in 2021, and patients found to harbor asymptomatic C. auris colonization tripled from 2020 to 2021 to over 4,000. In that same time frame, reports of drug resistant C. auris cases increased from 3 to 19. This is disastrous in a pathogen with a 30-60% case fatality rate, right?
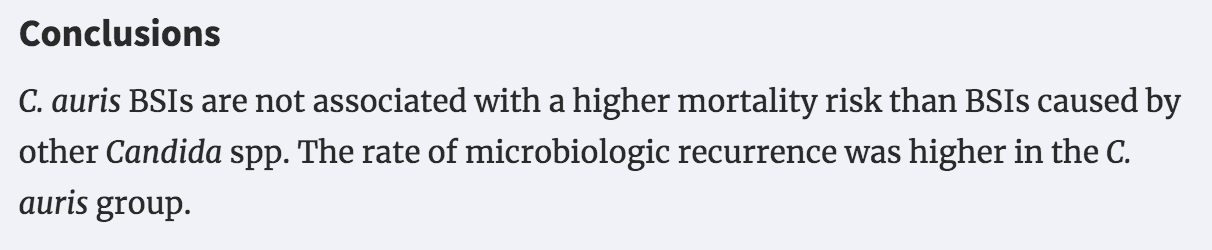
No, not really. Candida glabrata has the same approximate fatality rate. So, too, does that Candica albicans gifting you those unsightly yellow toenails. Any candidal infection once it gets into your blood stream is highly lethal, for the simple reason that people who die of systemic fungal infections are generally close to dying before their infection. People with minimally functional immune systems are almost always able to manage their fungal co-travelers safely. Athlete’s foot does not pose a mortal risk to most people; but if an elderly uncontrolled diabetic on dialysis gets some C. albicans through a fissure in their toes, things can get very hot very fast. Researchers in New York addressed this question directly, comparing outcomes in some 200 patients with systemic candidal infections, about half of whom had C. auris. While infections with C. auris were more likely to recur, they were no more lethal than other Candida species:
It’s hard to assess the degree to which Candida auris is spreading through the country at an “alarming” rate, as well. Lacking a commercial lab test, samples have to be sent to the CDC for testing, and the CDC has not released useful information on, say, positivity rates on random samples over time. It’s certainly possible that fewer physicians thought to test for C. auris in 2019 than 2021 given the relative lack of fuss until recently.
I’m game, though, to admit that this is probably an organism that is legitimately on the rise. In fact, I suspect this horse is probably well out of the barn.
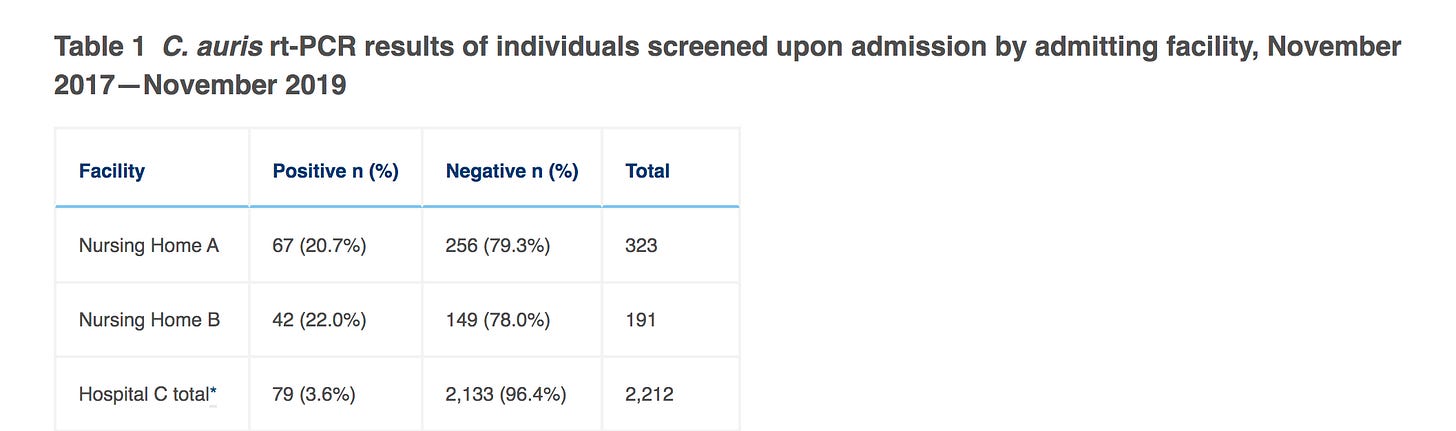
Going way back to 2017, a pilot screening program in New York City that ran until 2019 (yes, the year there were only 476 known cases in the entire nation), 20% of admissions to two nursing homes tested positive for C. auris on the skin of their armpits or groin, or in their nostrils. Twenty percent! Due to Medicare regulations, almost everyone heading to a nursing home is coming from a hospital, often with multiple recent hospital stays; a much lower but still significant proportion of hospital admissions (3%) tested positive on screening.
Bear in mind, this was 3-5 years ago, and we’re being told that cases keep doubling — at the minimum — every year. I think it’s a safe bet that if someone screened every asymptomatic nursing home admission for C. auris, we would be finding a whole lot of it. Most likely, results would be similarly alarming if we swabbed every hospital nurse or physician, and even random patients who’ve been moved from bed to bed. Of course, when nurses, doctors, and patients go home, they return to a less carefully cleaned environment, and most likely spread their new yeast colonizers to the skin of their loved ones. A fair question to ask, given the CDC recommendations for preventing transmission from asymptomatic carries of C. auris, is: “Do we really want to know?”
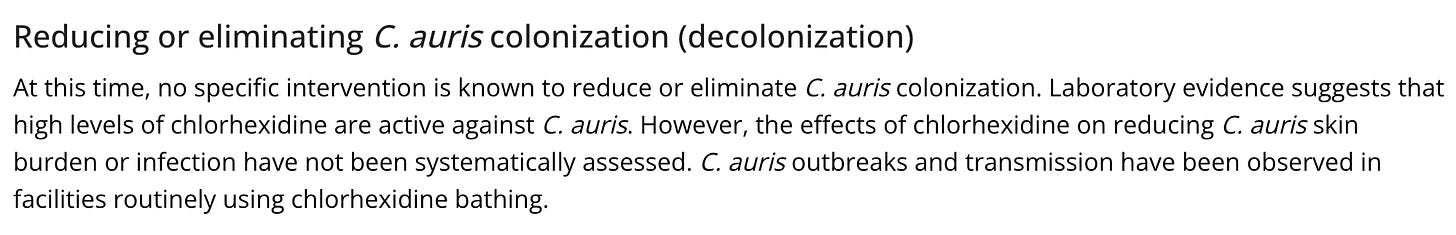
Aside from the burden that such a “diagnosis” places on hospitals and patients — yes, yellow suits, contact precautions, single rooms (or doubling up with other colonized patients), extra cleaning, etc. — there’s one other small problem. We don’t have a way to treat people colonized with this yeast, and it’s not clear that it goes away on its own:
I’m certain the CDC has learned its lessons from the Covid-19 pandemic, and will not make sweeping, disruptive recommendations without trying to gather some evidence first. Right? Given that it is not at all clear that trying to stop the spread of this microbe in hospitals will either reduce community-wide transmission, or change outcomes in our most frail inpatients, perhaps some hospital or nursing home systems could institute screening programs with aggressive interventions, and others could continue the status quo (no screening). After a couple years, we might see if there is a trend towards fewer cases of systemic C. auris infections or lower rates of positive screens on new hospital admissions in those with screening programs. That would be smart. I will not hold my breath.
As of now, this is what the CDC has given medical facilities by way of warning:
But what should that “continued surveillance” look like? Their document entitled, “Screening for Candida auris Colonization,” consists entirely of “consider",” “should consider,” and “should strongly consider” type recommendations, but no firm guidance. I don’t know what I would do if I were a hospital or skilled nursing facility administrator in the face of this concern. Start the suggested “point prevalence survey” and find myself a whole lot of C. auris to deal with? Only swab roommates or contacts of someone with a known case? Or just keep my head down and hope it doesn’t turn up in a patient on a ventilator? It’s not exactly guidance, perhaps because the CDC knows, deep down, that this is a problem they don’t really want to try to solve.
One other thing bears mention, though, since that Washington Post article was so over-the-top: the climate change angle. OK, I know climate change has joined politics and religion as poor dinner table conversation, but I cannot resist. The “opinion/hypothesis” piece cited by the Post that was run in 2019 by the American Society of Microbiology was just plain weird:
Without going deep into the weeds of global climate change or fungal evolution (neither a subject I wish to study at great length) I think most of us can agree that whatever is happening to global temperatures, it’s pretty unlikely that they moved in such pronounced lockstep on three continents (India, Venezuela, and South Africa were the countries where C. auris emerged) on the heels of the new millennium that this new threat was forged into existence simultaneously in those three far-flung places due to a modest increase in ambient temperature! Yes, it appears C. auris can thrive at a slightly higher temperature than other similar yeasts. However, human pathogens constantly mutate, very much including their genetic ability to survive and multiply in cooler or warmer hosts (fever being an excellent example of the host vs. pathogen warfare that goes on in this evolutionary battleground). We only find out about the mutations which worked. This one worked for C. auris. Good mutations tend to find their way forward, and SARS-CoV-2 has made it clear that often it’s impossible to figure out exactly how. There’s no need to conjure up fanciful theories — even if they help sell newspapers by adding one more black hat to global climate change — when more plausible ones exist.
So, no — I don’t think global warming is culpable for a super-bug fungus that will bring us waves of suffering and death. Candida auris is the latest yeast capable of causing severe infections in frail individuals, and I suspect its success in establishing itself in our communities will have more to do with its own qualities than our human responses to its arrival. As a physician, I’d love to see another class of anti-fungals emerge which could control serious infections from this pathogen; it’s a terrible feeling to helplessly watch a patient die for lack of the right drug. However, with many other lethal threats already lying in wait for our sickest patients, I also suspect that this particular yeast is unlikely to significantly increase the risk of death from a serious hospital stay.
I hope I am right on that last count. It might be years, or even decades, before the real impact of Candida auris is understood.
In the meanwhile, it’s fair to wonder if our latest public health threat has already carved out a nice home on your skin.
https://doctorbuzz.substack.com/p/has-climate-change-spawned-a-deadly


No comments:
Post a Comment
Note: Only a member of this blog may post a comment.