Matthew F. Watto, MD: Welcome back to The Curbsiders. I'm Dr Matthew Frank Watto, here with my great friend and America's primary care physician, Dr Paul Nelson Williams. Paul, what is MASLD?
Paul N. Williams, MD: MASLD is metabolic dysfunction–associated steatotic liver disease.
Watto: We talked about a really stripped-down way of testing people for MASLD. If we see mildly elevated liver enzymes, what should we be testing, and how does alcohol factor in?
Williams: Before you can make a definitive diagnosis of MASLD, you need to rule out other causes of liver inflammation — things that would cause a patient’s transaminases to increase. Alcohol is synergistic with everything that can harm the liver.
A great place to start is to gauge someone's alcohol intake to make sure it isn’t causing hepatic inflammation. The phosphatidyl ethanol level is a serologic test to determine chronic, heavy alcohol use. It's a new kid on the block. I've seen it mostly ordered by hepatologists. It is a way of determining whether someone has had fairly consistent alcohol use up to 4 weeks after the fact. The cutoff for a positive test is 20 ng/mL.
Dr Tapper frames the test this way. He isn’t using the test to catch someone in a lie about their alcohol use. He tells patients that he orders this test for all patients with liver inflammation, because alcohol is a common cause. The test helps him better understand the factors that might be affecting the patient’s liver function.
If the test comes back positive, you can have a conversation about that, and if it’s not positive, you move on to the next possible cause. Other fairly common causes of liver inflammation are relatively easy to address.
Watto: Instead of ordering ceruloplasmin or alpha-1 antitrypsin tests, for example, the first thing Dr Tapper recommends is checking for hepatitis B and C. We can cure hepatitis C. We can’t cure hepatitis B, but it’s important to know if the patient has it. Primary care physicians should be comfortable ordering these tests.
Really high ALT levels (eg, in the 200s) don’t usually happen from steatotic liver disease. In those cases, we would send an expanded panel that might include tests for autoimmune hepatitis-ANA, anti–smooth muscle antibody, and IgG levels. Otherwise, most of these patients don't need much more testing.
What is a FIB4 score and how does that factor in?
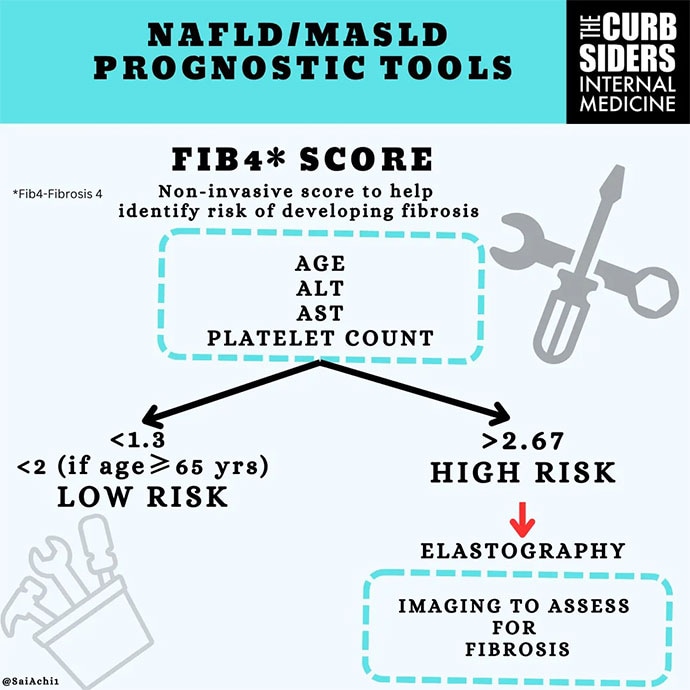
Williams: The FIB4 score estimates the degree of fibrosis based on the ALT and AST levels, platelet count, and the patient’s age. These data are plugged into a formula. If the FIB4 score is low (meaning not much fibrosis is present), you can stop there and do your counseling about lifestyle changes and address the reversible factors.
If the FIB4 score is above a certain threshold (1.3 in young adults and 2.0 in older adults), you need to find a more concrete way to determine the degree of fibrosis, typically through imaging.
Elastography can be done either with ultrasound or MRI. Ultrasound is typically ordered, but Dr Tapper recommends doing MRI on patients with a BMI > 40. Those patients are probably better served by doing MRI to determine the degree of liver fibrosis.
Watto: Patients with low FIB4 scores probably don't need elastography but those with high FIB4 scores do. For the interpretation of ultrasound-based elastography results, Dr Tapper gave us the "rule of 5s".
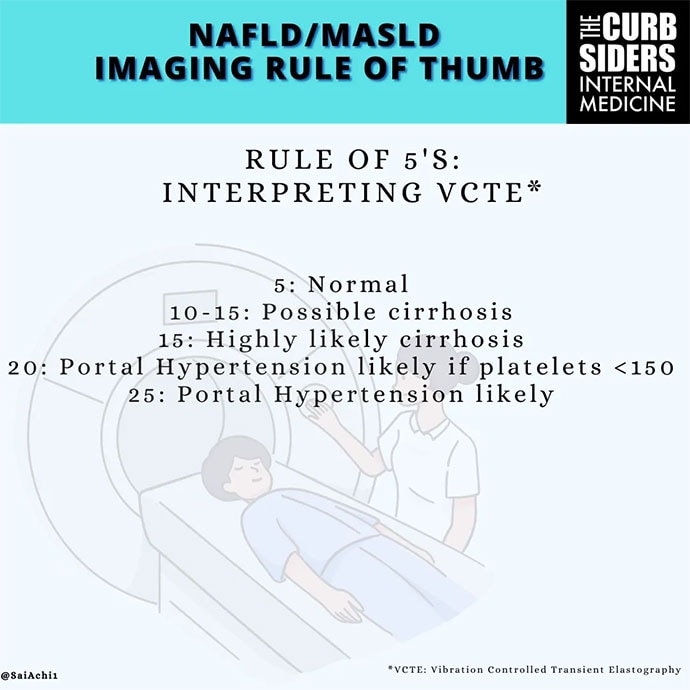
Elastography results are reported in kilopascal (kPa) units. A finding of 5 kPa or less is normal. Forty percent of those with a result of 10 kPa might have advanced liver disease. Above 15 kPa, the likelihood of cirrhosis is high, becoming very likely at 25 kPa. Finally, with a result of > 25 kPa, portal hypertension is likely, and you might need to have a conversation about starting the patient on medicine to prevent variceal bleeding.
We are moving toward more noninvasive testing and avoiding biopsies. We have cutoff values for MRI-based elastography as well. Both of these tests can help stage the liver.
What can we tell people about diet?
Williams: Weight loss is helpful. You can reverse fibrosis with weight loss. You can truly help your liver and bring it closer to its healthy baseline with weight loss. A loss of 7.5% body weight can reduce steatohepatitis, and with around 10% of body weight loss, you can actually resolve fibrosis, which is remarkable.
We all know that weight loss can be very therapeutic for many conditions. It's just very hard to achieve. As primary care doctors, we should use what we have in our armamentarium to achieve that goal. Often, that will include certain medications.
Watto: I like giving patients the 10% number because if they weigh 220 pounds, they need to lose 22 pounds. If they weigh 300 pounds, it's 30 pounds. Most people who weigh 300 pounds think they need to lose 100 pounds to have any sort of health benefit, but it’s much less than that. So, I do find that helpful.
But now a new drug has been approved. It's a thyroid memetic called resmetirom. It was from the MAESTRO-NASH trial. Without weight loss, it helped to reverse fibrosis.
This is going to be used more and more in the future. It's still being worked out exactly where the place is for that drug, so much so that Dr Tapper, as a liver expert, hadn't even had the chance to prescribe it yet. Of course, it was very recently approved.
https://www.medscape.com/viewarticle/most-common-chronic-liver-disease-world-2024a1000k1p
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.