It was the tail end of a cold Massachusetts winter when many of Dr. Larissa Lucas' nursing home residents stopped eating and drinking.
Others were sleeping more than usual, or especially groggy during their waking hours.
There were no high fevers or coughs – no obvious symptoms. And yet, starting in March 2020, Lucas would check on her residents and find they’d died quietly. A test result returned too late or a post-mortem swab would confirm it: they were positive for COVID-19.
Lucas marked the death certificates accordingly. Talking about it now, a rawness overcomes her throat.
“April through June, there was not a day that went by that I didn’t have a death certificate,” said Lucas, the medical director of extended care for North Shore Physicians Group in Peabody, Massachusetts.

All across the country, frontline staff in nursing homes saw the path the pandemic would take – isolation, fear and death. Health care workers in hospitals were inundated, exhausted. Coroners and medical examiners were working longer hours than ever before to keep up with the flood of bodies coming to their offices.
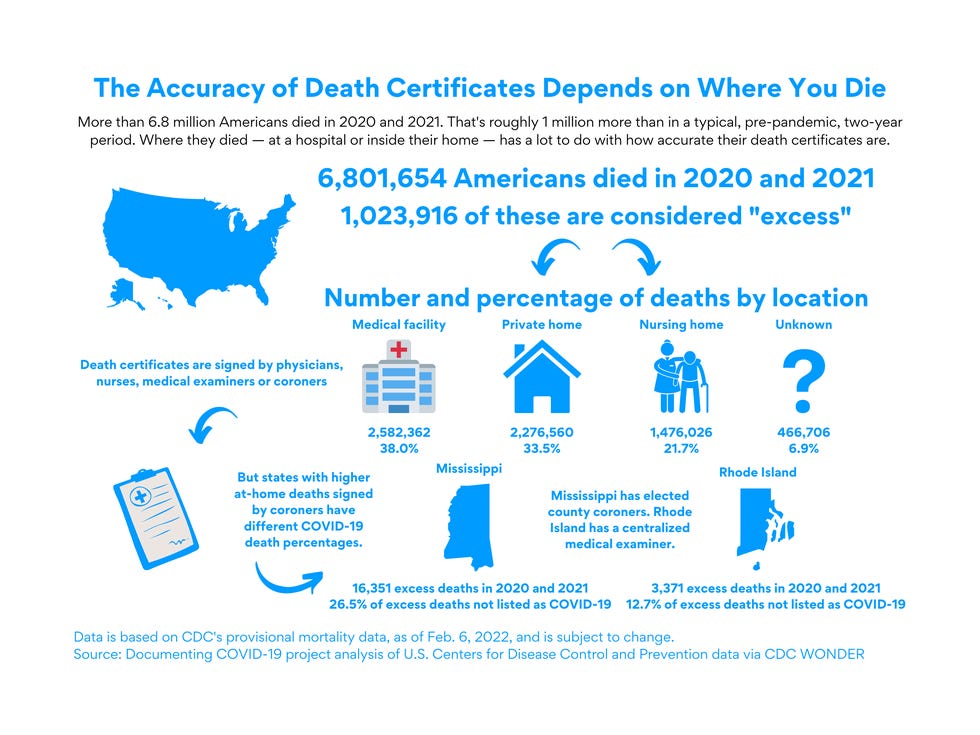
In every wave of the pandemic, a number of Americans who died of the virus didn’t have COVID-19 included on their death certificate. Their deaths instead were attributed to other causes — Alzheimer's disease, hypertension, heart failure. For this reason, the true number of COVID deaths could be up to 150,000 more than the official toll, experts suggest.
But in New England, something different happened.
How New England more accurately evaluated and counted COVID deaths
Death certificates can be filled out incorrectly for a multitude of reasons, including a lack of training for health care workers on how to investigate cause of death, few resources for post-mortem testing or autopsies and, in some cases, the willingness of certifiers to leave COVID off a death certificate at the family’s request.
The USA TODAY Network in New England and the Documenting COVID-19 project partnered to investigate how New England became a positive data anomaly in terms of COVID death reporting accuracy.
Across the region, excess deaths during the pandemic are almost completely accounted for by official COVID deaths, according to our analysis of Centers for Disease Control and Prevention mortality data and expected death models developed by demographers at Boston University. In other parts of the country, these COVID deaths were missed or certified incorrectly as other causes.
We investigated how New England did it. Here's what we found:
- During peaks of excess deaths – or more deaths than a normal, non-pandemic year – excess deaths in New England are logged as COVID deaths.
- The accuracy in COVID death reporting in New England stems from some of the best hospitals in the U.S.; well-run and funded public health departments; and state medical examiners who can act as a final check to ensure information on how and why New Englanders are dying is both accurate and timely.
- Higher reporting standards and more accurate data seem to have led to New England’s higher percentage of COVID deaths in nursing homes than almost anywhere else in the country, and in turn, paint a clearer picture of where COVID deaths happen.
- Since 2020, more than 1 million more people have died than normal, non-pandemic years. About 850,000 of those deaths are COVID deaths. The gap between is more than 200,000 "excess deaths," or deaths more than the historical baseline.
Deaths for other external reasons, such as homicide or drug overdose, did increase during the pandemic. But deaths from external causes resulted in 32,000 more deaths in 2020 than 2019, while deaths from natural causes resulted in 145,000 more. This means that the lion’s share of excess deaths are deaths from natural causes, many of which are diseases that become fatal when coupled with COVID-19.
The unexplained excess deaths attributed to causes other than COVID suggest an enormous undercount of COVID deaths across the country. In some counties, the true COVID death toll may be twice as high as the official number.
The difference between New England and many other parts of the country is that spikes in deaths during the pandemic align with COVID death totals.
Maine and Vermont partly defy this trend, but both states have had very low levels of COVID cases and hospitalizations throughout the pandemic along with large increases in deaths from overdoses, so it’s unlikely that missing excess deaths in these states are related to COVID-19.
This project explored the roles that two major systems in New England played in the region’s COVID death reporting – specifically state medical examiners and nursing homes.
Hospitals are a dominant and central data source to capture the pandemic’s death toll. But national data shows the country’s unexplained excess deaths aren’t typically coming from hospitals, as COVID’s role in death is clearer in these settings.
Connecticut Chief Medical Examiner Dr. James Gill said New England is “special,” in that all six states have cohesive, statewide systems to probe death. Centralized state medical examiners are appointed medical doctors and oftentimes also forensic pathologists. They’re not politically affiliated, like many elected county coroners elsewhere, and they oversee an entire state.
“You are really able to have a good handle on the investigations, and they’re all done in a similar fashion,” Gill said, noting he has a close working relationship with state public health officials.
Those factors combine to create a strong system of public health surveillance, as opposed to states where county coroners are elected without required experience and death investigation processes can vary wildly within just a few miles.
For the hundreds of thousands of people who died of COVID-19, where they lived and died likely had an influence on how their death was evaluated and recorded on their death certificates.
‘That is what took his life’
Lia Catanzaro’s father was recovering from a successful heart surgery at a Fall River, Massachusetts, hospital when he contracted COVID in June 2020.
A lifelong Rhode Island resident, Paul Catanzaro was 61 when he died. His death certificate lists COVID as the cause, a physical validation for his daughter in a world that seems to always be questioning her dad’s death.
“I think this is so important because that is what took his life,” she said, “regardless of any underlying conditions.”
People are often quick to point out the role of underlying conditions in an early death for someone with COVID, said Catanzaro, who lives in Cranston, Rhode Island. But her father could have lived well into his 80s with modern medicine, she believes. Instead, COVID ended his life prematurely, and his death certificate reflects that.
“I feel like we were very fortunate that his doctors actually recognized that,” Catanzaro said. “And I only say that now after being part of COVID support groups where I see people’s stories, that depending on certain situations or the area of the country, their loved ones don't have COVID on their death certificates.”
Vermont Chief Medical Examiner Dr. Elizabeth Bundock called death certificates “the foundation of the country’s mortality data.”
“It’s important not just for epidemiology, but it’s important for family members,” she said. “The cause of death, that’s important for current survivors and it could be important to someone the next generation away.”

Death certificate errors aren’t just a COVID problem, said Dr. Kathryn Pinneri, president of the National Association of Medical Examiners, one of two accrediting bodies in the U.S. Before the pandemic, it was estimated that one-third of death certificates contained errors.
But with the inconsistencies across systems, Pinneri said, it's "apparent how easy it is" to miss COVID deaths. And overreporting is “just as bad,” she said.
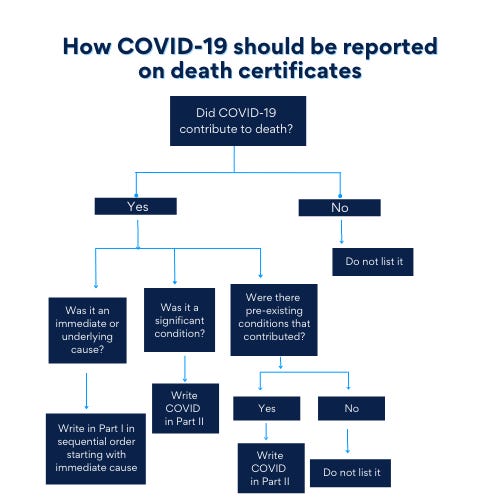
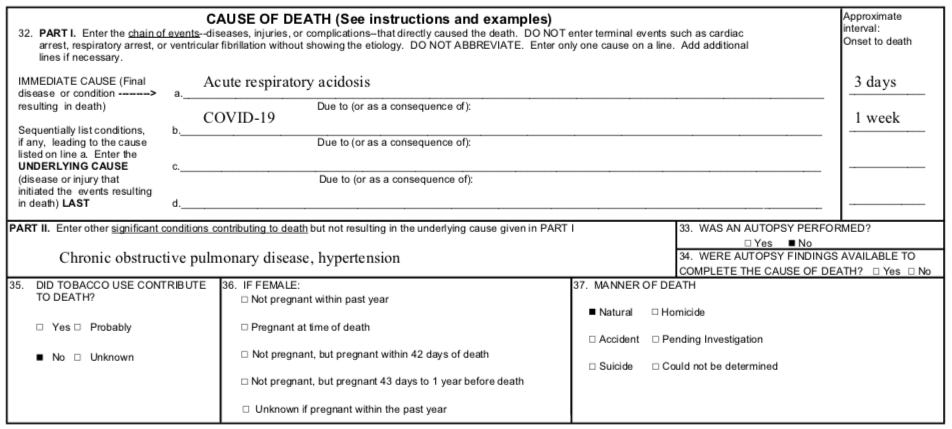
When COVID leads to death, it should be listed as the underlying cause of death, the CDC advises, as the virus can bring on conditions more likely to become the immediate cause. Death certifiers have to determine the chain of events leading to a death, and report that as accurately as possible on Part I of the certificate. If COVID is part of that sequence, the death should be counted as a “COVID death.”
The CDC instructs that any pre-existing condition that contributed to the death, but did not cause it, should be listed in a lower section, Part II, on the death certificate.
State medical examiners: A catch basin and clearinghouse of information
In a chilled, steel room at the University of Vermont Medical Center, Dr. Elizabeth Bundock works mostly alone, conducting autopsies, specimen collections and examinations. She spends her 9-to-5 with the deceased, while her community-based investigators tend to deaths across Vermont.
There are currently two job vacancies in the Vermont Chief Medical Examiner’s Office, reflecting staffing shortages plaguing the profession nationwide. Because it’s a small state, Bundock is tasked with reviewing every single death certificate in Vermont, which is unique for a medical examiner.
“It’s nice to get it right for someone at the end,” she said. “Birth certificates and death certificates, these could be the only two parts of their story captured. The story of their birth and the story of their death. Not all of us have our stories told.”

Centralized state medical examiners in New England play a critical role in death investigation both directly and indirectly. They directly investigate about 1 in 10 deaths in the region – usually deaths that happen for unnatural reasons, such as car accidents, drug overdoses or homicides. And though they almost never investigate deaths from natural causes, medical examiners do have to review and clear cremation cases, which encompass a large portion of natural deaths in New England.
But medical examiners in most New England states, except Massachusetts, are the final word for deaths related to a public health hazard, such as COVID. In states like Connecticut and Vermont, these highly skilled and trained professionals have a significant hand in proper data collection.
About 1,500 counties across the country have coroners handling death investigations as opposed to medical examiners. While medical examiners are certified doctors, coroners hold a political office that often requires no prior training or experience beyond proof of residence in the county. Medical examiners are usually appointed by state agencies, not elected.
According to the Documenting COVID-19 project's analysis of a recent Department of Justice survey of medical examiner and coroners' offices across the country, excluding Massachusetts who didn’t participate in the survey, New England medical examiners have more resources than coroners. The median total budget is $75,000 for a county coroner office, while state medical examiner offices in New England have a median budget of more than $2 million.
Though state medical examiners cover much larger populations than county coroners, the difference in budgets translates to about $300 more per case in New England. Coroners' budgets can vary widely. County coroners in Alabama average about $288 per case they accept, compared to New England’s $1,250 per case.
That additional funding means extra investigative muscle. Investigative ability is a major benefit of having a medical examiner involved in statewide data collection, said Connecticut’s Gill.
“A medical examiner is able to catch things that doctors can’t,” he said.
Gill and his investigators have proven just that. As of November 2021, they had gone to 308 funeral homes to conduct post-mortem swabbing in an effort to catch COVID deaths that nursing homes and hospitals may have missed. They were able to identify approximately 160 more that way, Gill said, and with the latest omicron surge, they are still in funeral homes every day.
In New Hampshire, from May 2020 to June 2021, Chief Medical Examiner Dr. Jennie Duval said her office routinely tested all deceased individuals under its jurisdiction, regardless of symptoms or cause of death. They also took deaths they normally wouldn’t have pre-pandemic – like natural deaths with evidence of a recent flu-like illness.
The CDC now advises that COVID testing “should be conducted whenever possible,” but certifiers can write “probable” or “presumed” COVID on the death certificate based on their best clinical judgment.
Gill said investigators take several factors into account when someone dies unexpectedly at home – the deceased’s vaccination status, conversations with next of kin and any symptoms that may have been present before death.
“If a person was not vaccinated and had been having shortness of breath the last few days, we’re going to bring that body in and do an investigation,” said Gill.
Also standing out in New England, medical examiners are conducting autopsies at a higher rate than much of the country. Autopsies have long been known as a gold standard for proper death investigation, and yet the rate at which they're done has decreased nationally over the years.
For these reasons, state medical examiners can serve as a “catch basin” of sorts for death certificates containing errors, and as a central clearinghouse of information for health care professionals.
Duval sent out universal guidancein the spring of 2020 to health care providers in New Hampshire about COVID death certification, offering lectures on the topic and access to an on-call 24/7 assistant medical examiner and pathologist.
Both Gill and Bundock detailed close relationships with their state vital records departments and epidemiology experts, including regularly double checking death certificates. They’re supposed to receive reports of all COVID deaths. That doesn’t always happen but verification efforts allow them to catch cases slipping through the cracks.
Reviewing the thousands of deaths slated for cremation each year is yet another way to catch a missed COVID case, Gill said. That process usually starts with a look at the death certificate and could lead to an investigation.
“It certainly gives us one more opportunity to identify a COVID death,” he said. “We have identified COVID deaths through this process.”

Like Gill, Bundock scrutinizes the death certificates her office receives. If something isn’t adding up, she may investigate further.
“It’s really the ones that don’t have an underlying etiology that we’re going to pursue a bit harder,” Bundock said. “When you have an elderly person with a complex medical history with multiple mechanisms going on for why they are dying, it can be hard to weigh one disease against another.”
In such cases, Bundock becomes what she termed a “Monday-morning quarterback.” But death certification is a hard gig for everyone involved – logistically and emotionally – no matter where they come in the process.
“It's difficult for me, too,” she said.
Reporting COVID deaths in nursing homes is ‘nuanced’
When the coronavirus first emerged, the U.S. Department of Health and Human Services was slow to give direction on death reporting. When that guidance came in April, it stated that COVID should be specified somewhere on a death certificate if it was suspected to have played a role in the person’s death.
That left a lot of discretion to those filing death certificates across a country without a single, unified system for recording death.
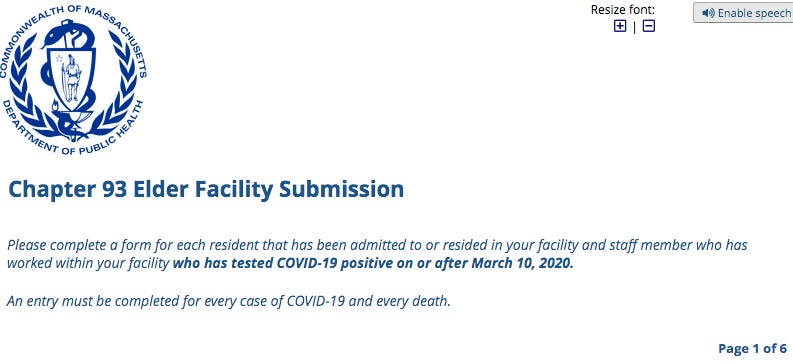
In some New England states, COVID death certifications are often later reviewed by medical examiners. But in Massachusetts, which does not have a public health hazard statute for its medical examiner, the state Department of Public Health maintains a central database for COVID surveillance information, called the Massachusetts Virtual Epidemiologic Network, known as MAVEN.
Via a REDcap reporting system, all Massachusetts long-term care facilities are required to report every COVID case and death to this database. The mandate came from state Legislature action following calls for transparency and the country’s deadliest nursing home outbreak at Soldiers’ Home in Holyoke in 2020.
The state has also gone back and checked previously recorded data against new reporting guidelines. In April 2021, a review led to a reduction in Massachusetts’ total COVID death toll by 1,220 deaths.
“I think there’s been a lot of data analysis and data cleansing that has taken place,” said Helen Magliozzi, director of regulatory affairs for the Massachusetts Senior Care Association, which represents nearly 400 facilities statewide.
Both Magliozzi and Dr. Larissa Lucas pointed to the state’s reporting mandate as a leading reason why Massachusetts nursing homes have been able to capture death data well.
At the group of nursing homes she works with on the North Shore, including Rosewood Nursing Home and Rehabilitation Center in Peabody, Lucas saw 100 deaths in the first 90 days of the pandemic. Normally, she would sign a handful of death certificates each month. But in those first three months, she signed that many in a single day.

In elder-care facilities, death certification is especially “nuanced,” said Lucas. Many residents are already dealing with various, compounding health conditions, teetering on the edge of decline.
“You could have scenarios where someone has advanced cancer and they get COVID, and you have to decide whether they died of the COVID infection,” Lucas said. “Did it push them over the edge, or did they die from the cancer they already had? That is a medical nuance that is really hard to capture.”
With the complication of comorbidities, Lucas said physicians strive to fill out death certificates with “a best faith opinion.” And it’s more than paperwork, she said. It’s an effort to give dignity and truth to someone’s passing.
“Death and dying is an incredibly sacred part of medicine,” said Lucas. “I believe how we leave this world is as important as how we enter it.”

Gill said in the early days of the pandemic, his office found death certificates from Connecticut nursing homes with non-specific causes of death, such as respiratory failure.
To correct potentially incorrect death certificates, Gill and his office went back and swabbed the deceased. This happened so often they were running through all the swabs they had.
“I was calling local hospitals begging, 'Can you give me 20 swabs?'” Gill said.
In both 2020 and 2021, states in New England reported higher percentages of COVID deaths in nursing homes than almost all other states. Efforts like Gill’s may be one key to why New England has reported COVID deaths more accurately than most of the country.
According to data from the Census Bureau’s American Community Survey, New England is home to some of the oldest populations in the country, but many other states with younger populations experienced higher increases in elderly and nursing home deaths during 2020 and 2021.
In other states, the difference is that fewer deaths were attributed to COVID on death certificates compared to New England.
Vermont, New Hampshire, Maine and Rhode Island lead the country in the percentage of COVID deaths in nursing homes since 2020. Yet the increase in nursing home deaths from all causes – including COVID, Alzheimer's disease and heart failure – pales in comparison to other states.

For families of those who have died of COVID, an inaccurate death certificate has several consequences: Families aren’t eligible for up to $9,000 guaranteed through FEMA’s COVID-19 funeral assistance program. Future generations won’t have documentation of the historical event that took a loved one from their family. And friends and family are left with the burden of finding closure to a death that can’t be easily explained.
On a recent February morning at Rosewood Nursing and Rehabilitation Center, standing in the halls carpeted with green and gold, geriatric nurse practitioner Sheela Kaithamattam welled with tears recalling her patients lost in the early days of the pandemic – and her phone calls to their families.
“I still can picture them,” she said, “my patients who would not have died if they didn’t have COVID.”
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.