First a review of the main trial then to the new paper in the Journal of the American College of Cardiology.
SELECT Trial
The SELECT trial was the first to show that the glucagon-like-peptide-1 receptor agonist (GLP1) semaglutide could actually modify cardiovascular disease. The discovery of another disease-modifying agent for heart disease is a breakthrough.
SELECT randomized more than 17,000 patients with cardiovascular disease and obesity but without diabetes to semaglutide or placebo. Semaglutide led to a 20% reduction in a composite primary endpoint of CV death, myocardial infarction or stroke. The hazard ratio was 0.80 and the 95% confidence intervals went from 0.72-0.90. The p-value was very low.
We say that this was a clinically important and statistically robust finding.
Now let’s notice a few things about the results.
First is the number of patients in the study. The authors did not enroll a few hundred or a few thousand. They enrolled 17,604 patients.
Next point: look at the number of primary outcome events. There were 569 events in the semaglutide arm vs 701 events in the placebo arm. That is a lot of events. The authors knew that it would take that many events to sort out signal from noise.
Third point: the authors knew that people would be interested in other outcomes besides the composite of CVD, MI and stroke. The problem with this is that one specific outcome will surely have fewer events than 3 combined. Fewer events means that there is a greater chance of detecting noise rather than signal.
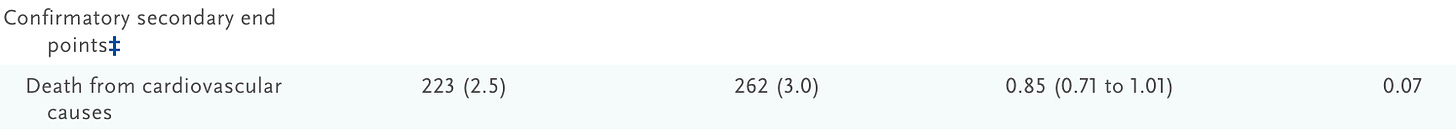
To account for mistaking noise and signal they used a rule: if the rate of death from cardiovascular causes was not statistically significant, then no other outcomes could be assessed. See the image:
The lower rate of cardiovascular death did not make statistical significance. The upper bound of the 95% confidence interval is more than 1.0 and the p-value is more than 0.05. All other outcomes below that (MI, stroke, death) were deemed “NA”.
The Dubious Substudy
For some reason, the authors of SELECT decided to break this rule and look at outcomes below CV death.
The outcome that made the title was COVID-19 related deaths. Sadly, the prominent journal JACC published the study.
They first separated out CV related and non-CV related deaths. Then they told us the most common cause of non-CV death was infections—62 vs 87, semaglutide vs placebo, respectively.
Then they went further. The trial was conducted during the pandemic and the authors collected data on infections and complications of infections.
Compared with placebo, semaglutide did not reduce the number of patients with a reported case of COVID-19 (2,108 vs 2,150 events; P = 0.46).
However, among patients who reported a diagnosis of COVID-19, fewer patients treated with semaglutide had serious COVID-19–related adverse events (232 [2.6%] vs 277 [3.1%]; P = 0.04).
They add this last sentence in the abstract:
High rates of infectious deaths occurred during the COVID-19 pandemic, with less infectious death in the semaglutide arm, and resulted in fewer participants in the placebo group being at risk for CV death.
Then in the conclusion there are these two sentences:
The lower rate of non-CV death with semaglutide was predominantly because of fewer infectious deaths. These findings highlight the effect of semaglutide on mortality across a broad population of patients with CV disease and obesity.
Comments
“Fewer infectious deaths” equals 62 vs 87. In a trial with 17,000 patients.
I hope that you can see how bad this is. In the main paper, to sort out the drug’s signal they recruited 17,000 patients, which then resulted in ≈ 1200 events. The authors then set out a rule that would prevent them from detecting noise. The rule was that CV death had to be significant to look further. It wasn’t, so they made no other claims about MI or stroke or all-cause death in the main paper.
Now they come out with a separate paper on infections—62 vs 87 events. And COVID-19 related adverse events—which they don’t describe, but number way less than then the total number of major adverse cardiac events.
All we get is one sentence in the limitations about testing subgroups may lead to underpowered analyses and chance findings. One sentence.
I highlight this study because it should never have happened. The authors broke their own rule about looking at low-frequency outcomes beyond the primary endpoint.
I am not sure I would go so far as saying this was p-hacking, but looking at data after you know the results and publishing positive findings is really problematic.
That the positive outcome had COVID-19 in it may have played a role in the study’s publication. It surely had a role in it being covered by 44 news outlets and Tweeted by hundreds of people—including some prominent MD-influencers.
Papers like this reduce trust in medical journals and scientists alike. I am not sure why medical scientists and journal editors can’t resist the urge to fly too close to the sun.
The SELECT trial was a huge win for cardiology. That should be enough.
John Mandrola--Heart rhythm doc, writer/podcaster for @Medscape, learner, cyclist, married to an #HPM doctor. #MedicalConservative. The more you see, the harder medicine gets
https://www.sensible-med.com/p/glp1a-drugs-are-great-but-unlikely

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.