Censorship in science shows up in numerous forms: ignoring, marginalizing, finding excuses, prioritizing, silencing — always in the name of rigorous science, of course. I provide here examples which I consider to be censorship of critiques that could have severely undermined the narrative of “safe and effective” Covid vaccines.
My examples are three “letters to the editor,” a format that allows unsolicited scientists to comment on a published article. Submitted to three leading medical journals, these letters pertained to studies from Israel about the effectiveness of the Pfizer vaccine. If accepted for publication, in most cases the authors would have been asked to respond. All three letters were rejected.
It is not easy to show censorship by a small series of rejected letters. Rejection messages contain only boilerplate text, and editors are protected by an obvious argument: They need to make difficult choices, given many submissions. Biased decision? Never!
Nonetheless, editorial decisions are not completely shielded from oversight. The merit of a rejected letter can be judged by other scientists, and sometimes by the layperson, too: Do my letters rank low or high on the merit scale? Do they raise minor points or major issues? Is their logic faulty or solid? Should all of them have been rejected, or rather – should any of them have been rejected?
Censorship or not?
You will be the judge.
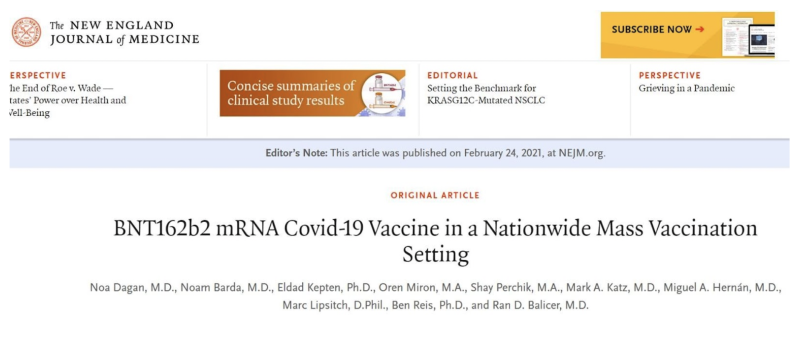
First letter (The New England Journal of Medicine, March 2021)
This was a one-paragraph letter, asking a simple question about two effects of the Pfizer vaccine, which were not reported in the article. Any remaining doubt about the importance of this question will dissipate after reading the last rejected letter.
To the Editor:
COVID-related death is subject to misclassification as is COVID-related hospitalization. Therefore, the study by Dagan et al. (1) on the effects of mRNA COVID-19 Vaccine should have included two crucial endpoints: all-cause death and any hospitalization.
It is of utmost importance to know the results of these analyses.
References:
- Dagan N, Barda N, Kepten E et al. BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Mass Vaccination Setting. N Engl J Med 2021; 384:1412–23
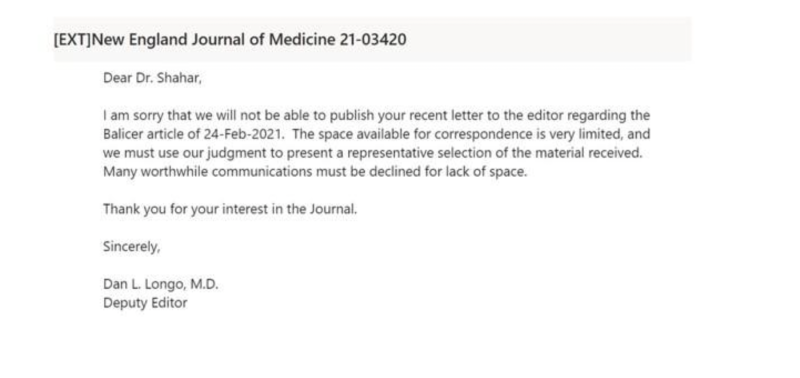
[The editor’s reference to “the Balicer article” is an (unusual) reference to the last author, rather than the first.]
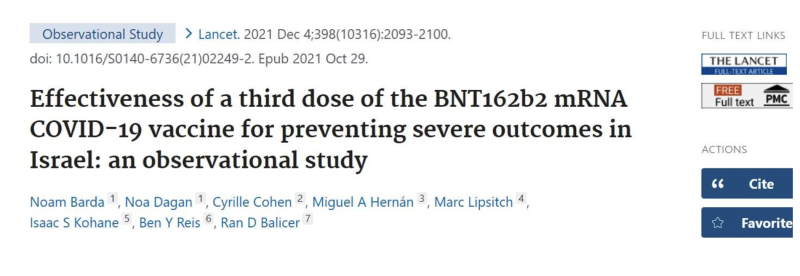
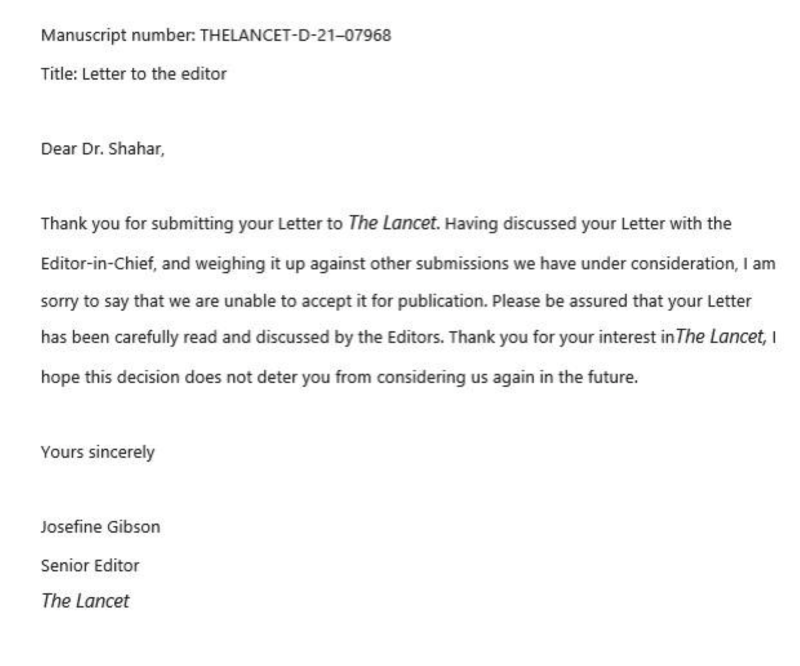
Second letter (The Lancet, October 2021)
This one is more technical, requiring some knowledge of research methodology. However, the basic idea is simple: authors should abide by their own methodological standards. Too much to ask for?
To the Editor:
The study by Barda and colleagues of a third dose of the BNT162b2 vaccine[1] excluded events that occurred during the first six days of follow up. The authors designed the study “to emulate a target trial”, but the methodological article they cite[2] (written by a co-author of Barda’s article) does not call for exclusion of early events. On the contrary, “With observational data, the best way to emulate time zero of the target trial is to define time zero to be the time when an eligible individual initiates a treatment strategy.”[2] What are the estimates when all events are included?
Although the study groups were carefully matched, residual confounding bias can never be excluded in observational research. One method to detect such bias employs “negative controls”, as eloquently explained by another co-author of Barda’s article.[3] In brief, researchers estimate the effect of the intervention on an outcome for which the effect is expected to be null. If the estimate is not null, residual confounding bias might also be present for the outcome of interest. For instance, “influenza vaccination was also “protective” against injury or trauma hospitalization…interpreted as evidence that some of the protection observed for pneumonia/influenza hospitalization or mortality was due to inadequately controlled confounding.”[3]
It is easy to apply the method to the study of Barda and colleagues:[1] What is the estimated effect of a third dose of the vaccine on non-COVID death, counting deaths as of day one? Is it null as expected? Of note, in a recent analysis COVID-19 vaccines showed unexpected “protection” against non-COVID mortality.[4]
References:
- Barda N, Dagan N, Cohen C et al. Effectiveness of a third dose of the BNT162b2 mRNA COVID-19 vaccine for preventing severe outcomes in Israel: an observational study. Lancet, October 29, 2021 DOI:https://doi.org/10.1016/S0140-6736(21)02249-2
- Hernán MA, Robins JM. Using big data to emulate a target trial when a randomized trial is not available. Am J Epidemiol 2016; 183(8): 758–64
- Lipsitch M, Tchetgen Tchetgen E, Cohen T. Negative controls: a tool for detecting confounding and bias in observational studies. Epidemiology. 2010;21(3):383–388
- Xu S, Huang R, Sy LS, et al. COVID-19 Vaccination and Non–COVID-19 Mortality Risk — Seven Integrated Health Care Organizations, United States, December 14, 2020–July 31, 2021. MMWR Morb Mortal Wkly Rep 2021;70:1520–1524.
Third letter (The British Medical Journal, June 2022)
This letter was submitted as a “Rapid Response” to a news item. There is no time limit for submitting a letter in a rapid-response format.
Title: Vaccine effectiveness studies from Israel suffered from severe misclassification bias of the mortality endpoint
Dear Editor,
“Real world” studies from Israel of vaccine effectiveness against death from COVID have relied on official classification of the cause of death during the vaccination campaign.[1, 2] We now have solid evidence that those studies suffered from 50% misclassification of the mortality endpoint.
The Israel Central Bureau of Statistics (CBS) estimated excess deaths versus COVID deaths in various periods. Between December 2020 and March 2021 — the first vaccination campaign — the ministry of health reported 3,298 COVID deaths in Israel, but CBS estimated only 1,641 excess deaths. The CBS graph and table can be found elsewhere.[3]
[You cannot include a figure in a Rapid Response. I provide it here, for your convenience.]
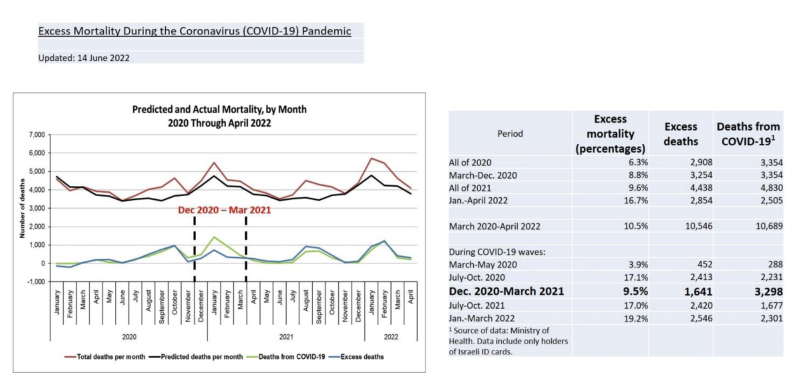
Evidently, half of reported COVID deaths at that time were not caused by COVID. They were part of background winter mortality in Israel, did not account for excess deaths, and could not have been prevented by a COVID vaccine. Therefore, those “real world” studies of vaccine effectiveness were subject to an unacceptable rate of misclassification of the mortality endpoint, and likely similar misclassification of correlated endpoints such as severe COVID and COVID hospitalization. As pointed out in an earlier response by Retsef Levi and Avi Wohl,[4] misclassification was probably differential (dependent on vaccination status).
Would reviewers have supported publication, had they known it back then?
References:
- Dagan N, Barda N, Kepten E et al. BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Mass Vaccination Setting. N Engl J Med 2021; 384:1412–23
- Hass, EJ, Angulo, FJ, McLaughlin, JM. et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalizations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data, Lancet, 2021; 397:1819–29
- Pfizer vaccine and COVID mortality: a call for retraction of publications from Israel
- Covid-19: Pfizer BioNTech vaccine reduced cases by 94% in Israel, shows peer reviewed study
The British Medical Journal does not inform authors about rejection of a “Rapid Response”. Below is part of their boilerplate message when a letter is received.
Enough time has passed. The letter was not published online. (Only posted responses might be selected for the printed journal.)
Three letters. Three journals. Three rejections.
Censorship or not? Did medical journals differ from the biased media?
Twenty-five years ago I published an article in the British Medical Journal in which I criticized the way letters to the editor had been treated.
Nothing has changed. Letters continue to be rejected without explicit, subject matter, justification. Editors can continue to dismiss any claim of biased judgment.
But now we have the internet. Rejected letters need not be buried forever, and editorial decisions can be judged in the public domain, like the case here. Perhaps some day we’ll even have an online, peer-reviewed journal titled The Journal of Rejected Letters. I am sure editors would prefer to not be featured there.
Dr. Eyal Shahar is a professor emeritus of public health in epidemiology and biostatistics. His research focuses on epidemiology and methodology. In recent years, Dr. Shahar has also made significant contributions to research methodology, especially in the domain of causal diagrams and biases.
https://brownstone.org/articles/the-censorship-of-covid-science-three-examples/
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.