Active shooter simulations can make emergency department staff feel more confident they’re prepared to respond to such a situation, according to a recent survey from a Texas children’s hospital.
Children’s Health Children’s Medical Center Dallas began hosting the simulations in August of 2016. In a survey of 204 staffers who underwent the voluntary training between August and December of that year, 92% said they felt more prepared and 70% said they were more knowledgeable about how to respond should a shooting occur.
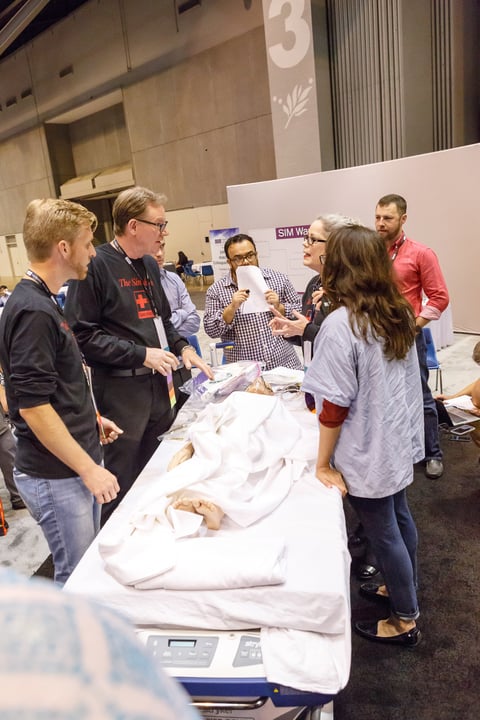
Participants undergo the training in the hospital’s simulation lab, which is set up to resemble the emergency department. Actors trained in crisis simulation are brought in, while hospital staffers remain in their normal roles, said Mary Baker, the survey’s co-author and a clinical educator at the hospital.
Conducting drills has become increasingly important at hospitals around the U.S. in light of growing concerns about mass casualty incidents, such as the shooting in Las Vegas last fall. But there are also growing concerns that hospitals themselves could become targets, such as with reports that suspects recently arrested at a New Mexico compound planned to attack Atlanta’s Grady Hospital. In 2014, the Department of Health and Human Services provided guidance on active shooting preparation for healthcare facilities.
The simulation forces participants to confront one of the basics of their training—patients and their safety first—since in the event of a shooting the staff members are encouraged to run and hide if they can, she said.
“That was probably one of the biggest things that came out of this,” Baker said. “There are people who said they couldn’t leave a teammate or patient if this was a real event.
How does it work
Ahead of the simulation itself, the participants are given an overview of the scenario and undergo some online preparation. Following the simulation, there’s a debriefing with all the simulation’s participants, including the actors.
All told, the entire training typically lasts between an hour and a half and two hours, Baker said.
Then, she said, the challenge becomes sustaining that education beyond that day of practice.
Children’s Medical Center Dallas, for example, has scheduled quarterly simulations to ensure new hires have an opportunity to undergo the training and to catch any staff members that need a refresher, she said.
“You can’t just do it once and be done,” Baker said.
The Emergency Nurses Association, which Baker is a member of, backs the program at Children’s Medical Center Dallas and works with others to promote and expand such projects. Groups like that can offer a significant tool for enhancing and sharing ideas on similar programs.
Another challenge is expanding the training program to also address issues that can arise when an emergency department is called to respond to treat people injured in a shooting or other mass casualty incident outside the hospital.
The volume of patients and the magnitude of their injuries can be extremely taxing on providers, and emergency plans must address that too, Baker said.
“In that kind of critical event, what we do for their moral distress [matters],” Baker said.
The Dallas hospital isn’t the only Children’s Health facility that’s done the active shooter training. Baker said it’s been implemented at another hospital, a rehabilitation facility and several clinics.
Integrating the drills into emergency training is something other health systems or providers can easily adopt—if they go about it thoughtfully, said Virginia Young, a clinical nurse specialist at Children’s Medical Center Dallas and another of the survey’s authors.
It’s crucial to have a strong grasp on the policy and regulatory implications in an active shooter situation and bring that to the training design, Young said. And if actors are involved, they need to have experience with simulations like these, as it can become a highly emotional experience for all involved.
Baker said that buy-in from the top down is another key to success since that can ensure programs can expand like Children’s did.
“It’s well worth your effort,” Young said, “it just needs to be planned out properly.”

