In April,
blood clots
emerged as one of the many mysterious symptoms attributed to Covid-19, a
disease that had initially been thought to largely affect the lungs in
the form of pneumonia. Quickly after came reports of young people dying
due to coronavirus-related strokes. Next it was Covid toes — painful red
or purple digits.
What do all of these symptoms have in common? An impairment in blood circulation. Add in the fact that
40% of deaths
from Covid-19 are related to cardiovascular complications, and the
disease starts to look like a vascular infection instead of a purely
respiratory one.
Months
into the pandemic, there is now a growing body of evidence to support
the theory that the novel coronavirus can infect blood vessels, which
could explain not only the high prevalence of blood clots, strokes, and
heart attacks, but also provide an answer for the diverse set of
head-to-toe symptoms that have emerged.
“All
these Covid-associated complications were a mystery. We see blood
clotting, we see kidney damage, we see inflammation of the heart, we see
stroke, we see encephalitis [swelling of the brain],” says William Li,
MD, president of the Angiogenesis Foundation. “A whole myriad of
seemingly unconnected phenomena that you do not normally see with SARS
or H1N1 or, frankly, most infectious diseases.”
“If
you start to put all of the data together that’s emerging, it turns out
that this virus is probably a vasculotropic virus, meaning that it
affects the [blood vessels],” says Mandeep Mehra, MD, medical director
of the Brigham and Women’s Hospital Heart and Vascular Center.
In a paper published in April in the scientific journal
The Lancet,
Mehra and a team of scientists discovered that the SARS-CoV-2 virus can
infect the endothelial cells that line the inside of blood vessels.
Endothelial cells protect the cardiovascular system, and they release
proteins that influence everything from blood clotting to the immune
response. In the paper, the scientists showed damage to endothelial
cells in the lungs, heart, kidneys, liver, and intestines in people with
Covid-19.
“The
concept that’s emerging is that this is not a respiratory illness
alone, this is a respiratory illness to start with, but it is actually a
vascular illness that kills people through its involvement of the
vasculature,” says Mehra.
A respiratory virus infecting blood cells and circulating through the body is virtually unheard of.
A one-of-a-kind respiratory virus
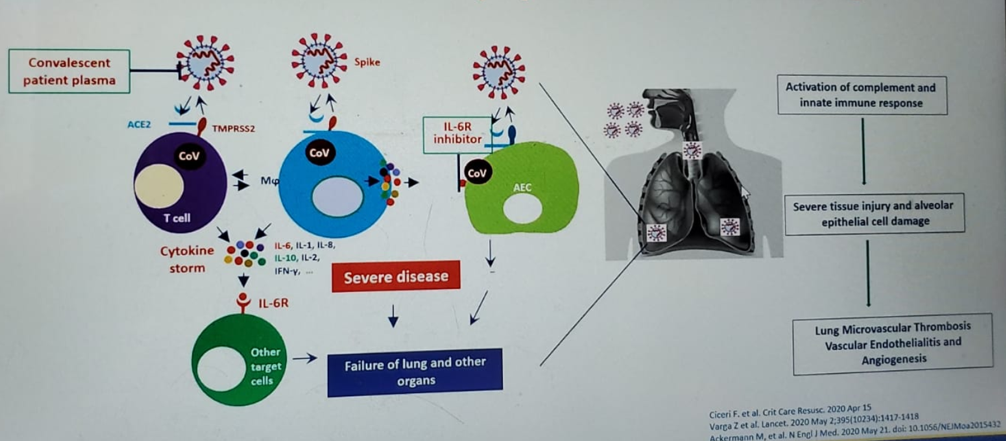
SARS-CoV-2
is thought to enter the body through ACE2 receptors present on the
surface of cells that line the respiratory tract in the nose and throat.
Once in the lungs, the virus appears to move from the alveoli, the air
sacs in the lung, into the blood vessels, which are also rich in ACE2
receptors.
“[The
virus] enters the lung, it destroys the lung tissue, and people start
coughing. The destruction of the lung tissue breaks open some blood
vessels,” Mehra explains. “Then it starts to infect endothelial cell
after endothelial cell, creates a local immune response, and inflames
the endothelium.”
A
respiratory virus infecting blood cells and circulating through the
body is virtually unheard of. Influenza viruses like H1N1 are not known
to do this, and the original SARS virus, a sister coronavirus to the
current infection, did not spread past the lung. Other types of viruses,
such as Ebola or Dengue, can damage endothelial cells, but they are
very different from viruses that typically infect the lungs.
Benhur
Lee, MD, a professor of microbiology at the Icahn School of Medicine at
Mount Sinai, says the difference between SARS and SARS-CoV-2 likely
stems from an extra protein each of the viruses requires to activate and
spread. Although both viruses dock onto cells through ACE2 receptors,
another protein is needed to crack open the virus so its genetic
material can get into the infected cell. The additional protein the
original SARS virus requires is only present in lung tissue, but the
protein for SARS-CoV-2 to activate is present in all cells, especially
endothelial cells.
“In
SARS1, the protein that’s required to cleave it is likely present only
in the lung environment, so that’s where it can replicate. To my
knowledge, it doesn’t really go systemic,” Lee says. “[SARS-CoV-2] is
cleaved by a protein called furin, and that’s a big danger because furin
is present in all our cells, it’s ubiquitous.”
Endothelial damage could explain the virus’ weird symptoms
An
infection of the blood vessels would explain many of the weird
tendencies of the novel coronavirus, like the high rates of blood clots.
Endothelial cells help regulate clot formation by sending out proteins
that turn the coagulation system on or off. The cells also help ensure
that blood flows smoothly and doesn’t get caught on any rough edges on
the blood vessel walls.
“The
endothelial cell layer is in part responsible for [clot] regulation, it
inhibits clot formation through a variety of ways,” says Sanjum Sethi,
MD, MPH, an interventional cardiologist at Columbia University Irving
Medical Center. “If that’s disrupted, you could see why that may
potentially promote clot formation.”
Endothelial
damage might account for the high rates of cardiovascular damage and
seemingly spontaneous heart attacks in people with Covid-19, too. Damage
to endothelial cells causes inflammation in the blood vessels, and that
can cause any plaque that’s accumulated to rupture, causing a heart
attack. This means anyone who has plaque in their blood vessels that
might normally have remained stable or been controlled with medication
is suddenly at a much higher risk for a heart attack.
“Inflammation
and endothelial dysfunction promote plaque rupture,” Sethi says.
“Endothelial dysfunction is linked towards worse heart outcomes, in
particular myocardial infarction or heart attack.”
Blood
vessel damage could also explain why people with pre-existing
conditions like high blood pressure, high cholesterol, diabetes, and
heart disease are at a higher risk for severe complications from a virus
that’s supposed to just infect the lungs. All of those diseases cause
endothelial cell dysfunction, and the additional damage and inflammation
in the blood vessels caused by the infection could push them over the
edge and cause serious problems.
The
theory could even solve the mystery of why ventilation often isn’t
enough to help many Covid-19 patients breathe better. Moving air into
the lungs, which ventilators help with, is only one part of the
equation. The exchange of oxygen and carbon dioxide in the blood is just
as important to provide the rest of the body with oxygen, and that
process relies on functioning blood vessels in the lungs.
“If
you have blood clots within the blood vessels that are required for
complete oxygen exchange, even if you’re moving air in and out of the
airways, [if] the circulation is blocked, the full benefits of
mechanical ventilatory support are somewhat thwarted,” says Li.
A new paper published last week in the
New England Journal of Medicine,
on which Li is a co-author, found widespread evidence of blood clots
and infection in the endothelial cells in the lungs of people who died
from Covid-19. This was in stark contrast to people who died from H1N1,
who had nine times fewer blood clots in the lungs. Even the structure of
the blood vessels was different in the Covid-19 lungs, with many more
new branches that likely formed after the original blood vessels were
damaged.
“We
saw blood clots everywhere,” Li says. “We were observing virus
particles filling up the endothelial cell like filling up a gumball
machine. The endothelial cell swells and the cell membrane starts to
break down, and now you have a layer of injured endothelium.”
Finally,
infection of the blood vessels may be how the virus travels through the
body and infects other organs — something that’s atypical of
respiratory infections.
“Endothelial
cells connect the entire circulation [system], 60,000 miles worth of
blood vessels throughout our body,” says Li. “Is this one way that
Covid-19 can impact the brain, the heart, the Covid toe? Does SARS-CoV-2
traffic itself through the endothelial cells or get into the
bloodstream this way? We don’t know the answer to that.”
In another
paper that looked at nearly 9,000 people with Covid-19, Mehra showed
that the use of statins and ACE inhibitors were linked to higher rates
of survival.
If Covid-19 is a vascular disease, the best antiviral therapy might not be antiviral therapy
An
alternative theory is that the blood clotting and symptoms in other
organs are caused by inflammation in the body due to an over-reactive
immune response — the so-called cytokine storm. This inflammatory
reaction can occur in other respiratory illnesses and severe cases of
pneumonia, which is why the initial reports of blood clots, heart
complications, and neurological symptoms didn’t sound the alarm bells.
However, the magnitude of the problems seen with Covid-19 appear to go
beyond the inflammation experienced in other respiratory infections.
“There
is some increased propensity, we think, of clotting happening with
these [other] viruses. I think inflammation in general promotes that,”
Sethi says. “Is this over and above or unique for SARS-CoV-2, or is that
just because [the infection] is just that much more severe? I think
those are all really good questions that unfortunately we don’t have the
answer to yet.”
Anecdotally,
Sethi says the number of requests he received as the director of the
pulmonary embolism response team, which deals with blood clots in the
lungs, in April 2020 was two to three times the number in April 2019.
The question he’s now trying to answer is whether that’s because there
were simply more patients at the hospital during that month, the peak of
the pandemic, or if Covid-19 patients really do have a higher risk for
blood clots.
“I
suspect from what we see and what our preliminary data show is that
this virus has an additional risk factor for blood clots, but I can’t
prove that yet,” Sethi says.
The
good news is that if Covid-19 is a vascular disease, there are existing
drugs that can help protect against endothelial cell damage. In another
New England Journal of Medicine
paper that looked at nearly 9,000 people with Covid-19, Mehra showed
that the use of statins and ACE inhibitors were linked to higher rates
of survival. Statins reduce the risk of heart attacks not only by
lowering cholesterol or preventing plaque, they also stabilize existing
plaque, meaning they’re less likely to rupture if someone is on the
drugs.
“It
turns out that both statins and ACE inhibitors are extremely protective
on vascular dysfunction,” Mehra says. “Most of their benefit in the
continuum of cardiovascular illness — be it high blood pressure, be it
stroke, be it heart attack, be it arrhythmia, be it heart failure — in
any situation the mechanism by which they protect the cardiovascular
system starts with their ability to stabilize the endothelial cells.”
Mehra
continues, “What we’re saying is that maybe the best antiviral therapy
is not actually an antiviral therapy. The best therapy might actually be
a drug that stabilizes the vascular endothelial. We’re building a
drastically different concept.”
https://elemental.medium.com/coronavirus-may-be-a-blood-vessel-disease-which-explains-everything-2c4032481ab2