In a remote fishing lodge in Soldotna, Alaska—a town of just over 4000 people along 2 million pristine acres of protected wilderness—Dr Robert Ledda leads a specialized medical practice designed to help his patients manage or even optimize aging. People travel here with a wish list that seems endless: more energy, less stress, a sharper brain, a stronger libido, a healthier heart, more resilient muscles and bones, a better immune system, a more youthful appearance.
The problem with “mainstream medicine,” says Ledda, is that it’s disease-oriented and reactive, not preventive: That is, nurses and physicians see patients when they’re sick, not sooner.
“They don’t have the time,” says Ledda, a partner with
Cenegenics Alaska, a branch of Cenegenics Medical Institute. Most doctors can’t spend 8 hours the first time they see a patient, as he does, evaluating activity levels, family history, stress, and eating habits. “They know that the vast majority of people are not going to change the way they live, so their tool bag is strictly disease-model and medication-based.”
In its marketing materials online and
on social media, Cenegenics claims its elite, pricey program—or “healthy aging plan”—will “reverse the declines of aging and protect your future health.” Cenegenics clinics worldwide offer the same promise, from
Boston to
Columbus, Ohio, to
Karnataka, India.
Physicians who specialize in so-called anti-aging medicine have long operated on the outskirts of the medical profession, and they draw their share of criticism, particularly for prescribing hormone therapy.
On a website called
HGH Watch, longevity expert Thomas Perls, MD, MPH, characterizes the prescribing of human growth hormone (HGH) for anti-aging as “quackery and hucksterism.” Perls, a professor of medicine at the Boston University School of Medicine, also writes that
hormone replacement therapy“and the drugs used to treat their side effects end up being hormonal toxic soups that can cause great medical and financial harm that far outweighs any long-term benefit.”
But as physicians brace for growing numbers of aging patients who hope to live longer and have a better quality of life in their older years with less disease, some treatments previously waved off as too emerging, expensive, or even vain are slowly becoming more accepted. The idea is that aging is inevitable, yes, but it’s also treatable—and even somewhat preventable.
“There’s way more scientists who are coming around [and] agree with our approach of primary prevention,” says Ledda, whose
certification in age management medicine is a credential that is not recognized by mainstream medicine.
Still, the ranks of doctors who practice anti-aging and age management medicine are growing. The
American Academy of Anti-Aging Medicine—which states its mission is to support research and technology that will “detect, treat, and prevent diseases associated with aging,” as well as treatments “designed to prolong the human life span” and “optimize the human aging process”—now has over 26,000 members. Of these, 85% are physicians and 12% are researchers, scientists, and “health practitioners.” (The remaining 3% is a mix of people, including members of the public.)
‘Specializing’ Without a Specialty
The question is, are these interventions that claim to combat the effects of aging based in science? Critics argue that the anecdotes and testimonials don’t pass the rigorous standards set by evidence-based medicine. Without clinical trials, the purported effects aren’t measurable or proven by legitimate science.
“Most of traditional medicine has taken a negative stance, I would say, against these [anti-aging interventions] because again, does it work? And is it safe? We can’t answer those questions,” says Dr Cynthia Stuenkel, a clinical professor of medicine at the University of California, San Diego, who published
a warning about compounded bioidentical hormone therapy in
JAMA Internal Medicine in 2017. Stuenkel also chaired the Endocrine Society’s
treatment guidelines for
menopause in November 2015.
The
American Board of Medical Specialties (ABMS) does not certify a specialty or subspecialty for anti-aging. “[Our] process to establish a new specialty or subspecialty is rigorous and thoughtful,” ABMS said in a statement. “It involves input from internal and external stakeholders, public comment, committee review, and is ultimately an ABMS Board decision.” To qualify as a specialty, the area of medicine must focus on a “distinct and definable” group of patients, a “definable type of care need,” a “stand-alone” set of medical knowledge, or “unique care principles,” as well as “clearly demonstrating its value in improving access, quality, and coordination of care.”
“I’m not worried about them infiltrating legitimate medicine,” says S. Jay Olshansky, PhD, a gerontology professor at the University of Illinois at Chicago School of Public Health.
“The fact that there is no medical specialty called ‘anti-aging medicine’ is all that you need to know,” Olshansky says. “This has been the case from day one. Nothing’s changed.” On the other hand, he applauds the efforts of “anti-aging” doctors who encourage their patients to adopt a healthier lifestyle.
“Does that modulate some of the effects of aging? Yes, of course,” he says. “If you exercise, eat right, and lose weight, chances are you’re going to feel better, and you’ll probably live healthier for a longer time period. So if that’s what you’re doing, and you’re calling yourself an anti-aging doctor, then there’s a legitimate element to what you’re doing.”
Focusing on Prevention

Robert Ledda, MD
With the exception of one crucial component of his practice—prescribing hormones—Ledda’s strategy for his patients is largely preventive, beginning with a $2500 evaluation day that generates a baseline report. Then, patients begin a program of consistent exercise, a low-glycemic diet, hormone manipulation, and a handful of daily supplements. The first annual visit costs $2495, and subsequent check-ups are $1995. The monthly program fee in the first year is $350, plus the costs of the supplements, hormones, and lab work.
Ledda shares the story of his aunt, Pam, who hadn’t seen a doctor in 3 years when she first visited his practice. The “before” photo on his clinic’s Facebook page shows a 60-year-old woman with a sweet smile and a mix of gray and golden brown hair. The scale told a different story: At 209 pounds, she was morbidly
obese.
“You go to a regular disease-model doctor, you’re going out the door on a blood pressure medicine, a cholesterol medicine, and a diabetes medicine,” Ledda says he remembers thinking after reviewing her first set of lab work. “The disease-model recipe was to start
insulin. So we’re talking real disease here.”
Gradually, Pam began to feel motivated to change. She started attending Ledda’s lecture series, and she also worked with Ledda’s low-glycemic (“paleo”) chef for a week to learn how to cook.
One motivator that works for many patients is fear, Ledda says. “I can create some fear that’s a little more concrete than, Someday I may have problems, but right now I just want to eat the cake. The challenge with every patient is really getting a hold of their psyche to the point where they realize they just can’t keep doing that.”
That fear transformed his aunt’s life, he says: She changed what she ate and began exercising in a CrossFit gym 3 days per week, and she lost a significant amount of weight. Now, she is more fit and feels better. “She’s had improvements subjectively in every domain you could think of, and all of her numbers are great. Her systemic inflammation went away,” Ledda says. In her “after” photo posted on Facebook, she is far thinner, in workout gear: a beige hoodie, sneakers, and tight black leggings. She’s standing with a pal outside a big wall emblazoned with graffiti, with a wide, confident smile.
Though Ledda says he put her on some “conventional meds” for high cholesterol and diabetes after her initial visit, he has now “taken her off almost everything”; now, “she has no metabolic disease at all,” no diabetes, and her “cholesterol panel is immaculate on no medicines.”
At her first visit, Pam’s total cholesterol was 280 mg/dL; her bad cholesterol was 200, and her good cholesterol was quite low, in the 30s. Ledda attributes the transformation to a handful of things working together: diet, supplements, lifestyle changes, and weight loss. Now, she takes 500 mg of
metformin daily, as well as a number of nutritional supplements. She’s also on hormone replacement therapy.
Changing the Hormonal ‘Soup’
Perhaps the most controversial element of the Cenegenics program is its focus on manipulating hormones in the aging body.
The regimen for women can include potentially dangerous bioidentical compounds, whereas men may be offered
testosterone HGH, which has not approved by the US Food and Drug Administration (FDA) for anti-aging purposes. HGH has only been cleared for use in patients with
HIV and for a rare condition in children called “adult growth hormone deficiency,” a diagnosis that has proved to be popular among anti-aging doctors.
Women who experience early or surgical menopause typically experience poorer cardiovascular, bone-density, and cognitive outcomes, as well as an increased risk of developing diabetes, Ledda says, which is why they are advised to undergo hormone replacement therapy. It can help most women who go through menopause.
“Why not continue them longer to continue to get those obvious benefits that science suggests are there?” he asks.
The Endocrine Society has come out against the use of HGH except in patients with clearly defined evidence of a growth hormone deficiency, Stuenkel says—for example, if they had a
pituitary tumor or hypothalamic dysfunction. Another hormone to watch out for, she adds, is dehydroepiandrosterone (DHEA), an adrenal androgen male hormone. It’s controversial because of the lack of good evidence supporting its use.
New Use for an Old Drug?
One potentially promising drug that has already been tested in millions of patients is metformin, a diabetes medication that some of Ledda’s patients—including his aunt Pam—take to manage
insulin resistance. “Ultimately, over many years of studying with tens of thousands of patients, we will learn if those people are healthier for longer—and then, we’ll have our first evidence that we’re on the right path,” says David Sinclair, a longevity researcher at Harvard who serves as an advisor for several biotech projects.
Patients who have taken the drug have less cancer, less heart disease, and less frailty than the average population, an effect that is “firmly based in science,” Sinclair says. “But because aging isn’t considered a disease, and you’re not diabetic until you actually have high blood sugar, you can’t easily get metformin as a preventive measure,” he adds.
The next step, Sinclair says, is securing funding to launch a massive study to test its safety and efficacy: the
Targeting Aging with Metformin (TAME) trial, led by Albert Einstein College of Medicine’s
Dr Nir Barzilai, who previously conducted the
Metformin in Longevity (MILES) study. The National Institutes of Health rejected its grant proposal last fall, but if the trial gets off the ground, researchers will follow 3000 patients who are between 65 and 79 years old. The trial has support from the
American Federation for Aging Research, and researchers hope it will show the FDA that aging can be slowed, and therefore can be treated as a medical condition, Sinclair says.
“Metformin could be the first drug that would be given to people in their 50s and 60s before they get sick, whereas now we wait until it’s too late.”
In the meantime, experts such as gerontology professor Olshansky remain skeptical about doctors promising to turn back the clock with “anti-aging” treatments that have not been proven effective.
“Mainstream medicine has not accepted this premise,” he says.
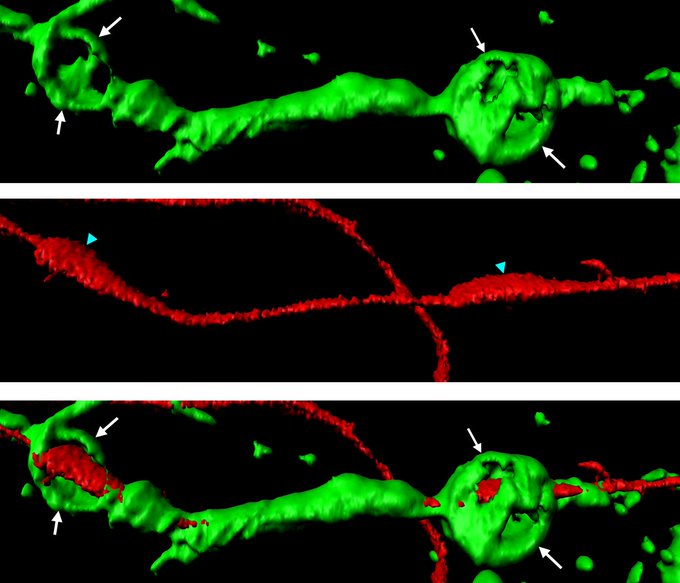

 | First step to induce self-repair in the central nervous system. The research team led by Prof. Claire Jacob
| First step to induce self-repair in the central nervous system. The research team led by Prof. Claire Jacob 